by Zachary Hafez MD & Melissa Kroll MD
expert reviewed by Hawnwan Philip Moy MD (@pecpodcast)
It\’s a slow Saturday morning and you as the medical director are riding out enjoying the unusually warm 60 degree weather…in February no less! To celebrate, you decide to visit your favorite coffee shop and get the world\’s best latte. Just as you pull in, dispatch suddenly pages out a 58-year-old male in cardiac arrest. It looks like your coffee is going to have to wait…but don\’t worry, you\’ll be receiving your daily dose of adrenaline soon.
When you arrive 5 minutes later, the first responders and paramedics are already hard at work pit crewing away. On an initial survey, you notice an odd appearing plastic device with flashing lights. Having read about them before, you ask your first responder where the Impedance Threshold Device (ITD) came from? Apparently, one of your Emergency Medical Response Agencies (EMRAs) is trialing ITDs. “We got a pulse!” exclaims one of your medics. As everyone breaths a sigh of relief, your fire first responder wipes her brow and asks, “So doc…what do you think of the ITD?” Before answering, you quickly try to buy some time by helping your crews prepare for transport and scramble to recount the evidence behind ITDs and cardiac arrest…

Background
In 1960 the American Heart Association (AHA) introduced cardiopulmonary resuscitation (CPR) to physicians and thereby becoming the premier educator in CPR training. Despite multiple advances in ACLS over the last 50 years, only modest improvement in survival rates have been achieved. In 2011, EMS responded to over 326,000 out-of-hospital cardiac arrests in the United States with a survival to hospital discharge of only 10.6% [1].
The reason for the lack of improvements in survival is multifactorial. Standard CPR is inherently less effective than a beating heart providing less than 25% of normal blood flow to the heart and brain [2]. Furthermore, the resuscitation is often limited by inadequate CPR, namely incomplete chest compression and chest recoil [3, 4, 5]. One of the more recent developments to augment the effect of CPR is the impedance threshold device (ITD).
Physiology of CPR and the Role of the ITD
The goal of CPR is to circulate blood from the heart to the body during chest compression and allow return of blood back to the heart during chest recoil. There are two predominantly accepted theories that explain how this may occur [6]. The first is the “cardiac pump theory” which is based on the principle that the heart is compressed between the sternum and vertebral column leading to mechanical ejection of the blood from the heart [7]. The second is the “thoracic pump theory” which is based on the principle that the thoracic cavity is a confined space whereby compression of the chest wall leads to an increase in intrathoracic pressure that causes ejection of blood from the heart into the systemic circulation and expiration of air from the lungs [8]. Decompression of the chest wall (i.e. natural chest recoil) leads to a decrease in intrathoracic pressure, resulting in venous return of blood. However, the hemodynamic gradient of the vacuum is attenuated by passive inspiration of air that occurs with chest recoil.
The ITD is designed to limit this passive inspiration of air during CPR. It is a disposable, plastic, cylindrical shaped device containing a silicon diaphragm which works as a one-way valve that can be attached to an endotracheal tube, laryngeal mask airway, or bag valve mask in line with the airway circuit. During chest compression, intrathoracic pressure becomes higher than atmospheric pressure opening the unidirectional valve and air is freely expired from the lung. During chest recoil, the intrathoracic pressure falls below atmospheric pressure leading to valve closure. A closed valve prevents air in the airway circuit from re-entering the lungs preserving a negatively pressured intrathoracic cavity.
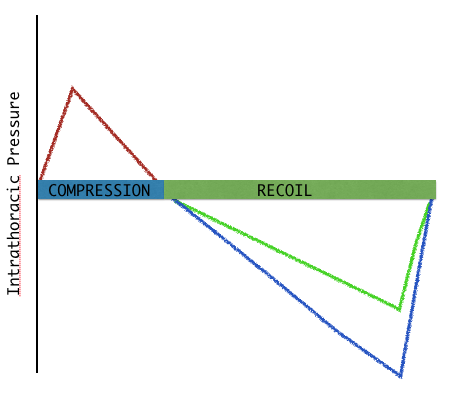

Creating a negatively pressured intrathoracic cavity, potentially leads to two primary circulatory benefits. First, the vacuum within the chest enhances venous return to the right side of the heart, which leads to increases in preload, systolic blood pressure, circulation, and ultimately priming the heart for the next compression. Second, use of the ITD reduces intracranial pressures more rapidly and to a greater degree during the decompression phase of CPR by maintaining lower intrathoracic pressures. This provides less resistance to cerebral perfusion during the next compression5. This leads to improved perfusion of the brain.
Literature Review
In 1995, Lurie demonstrated that the use of ITDs with CPR improved coronary perfusion pressures and a decreased in the number of defibrillation during resuscitation of swine models [9]. Even though the study only included 15 animals, it prompted discussion and future studies on the applicability of ITDs in cardiac arrest resuscitations Later, Mader et al performed a blinded, randomized controlled study with swine models. This study demonstrated that ITDs improved both coronary perfusion pressure and ventilation as measured by PaCO2, PaO2, and arterial pressures of the chest during standard CPR [10]. However, not all studies showed benefits associated with the use of an ITD. A study performed by Menegazzi et. al, unfortunately discovered that by adding ITDs to their standard CPR, there was a reduced survival rate of ventricular tachycardia in 36 randomized pigs (33% survival in the pigs that were revived with an ITD compared to 78% in pigs who were revived with standard CPR practices) [11].
Complicating the issue further was the inclusion of active CPR (compression-decompression) compared to standard CPR in subsequent ITD studies. Active CPR was first researched after a man successfully performed high-quality CPR with a plunger at home during a cardiac arrest. It is believed that during active CPR, forced recoiling of the chest wall increases the negative pressure in the intrathoracic cavity and, in effect, improving venous blood return. Thus, adding an ITD to active CPR would further potentiate a negative intrathoracic pressure and increase blood return. The combination of Active CPR with ITDs was first studied by Shih et. al. by using ITDs in conjunction with a novel adhesive glove device to provide active CPR on swine models. While the adhesive glove CPR improved flow with active compression-decompression, this study concluded that the addition of an ITD to the adhesive glove CPR had no statistical difference in perfusion compared to the adhesive glove CPR alone [12].
Despite Shih’s findings, Plaisance continued Shih’s thought process by studying ITD use with active CPR in human resuscitations. In 2000, Plaisance et al completed a prospective, randomized, blinded trial to compare active CPR to active CPR with the use of ITD [13]. Their use of the sham ITD allowed for blinding of the subjects and became the basis for most future blinded studies. The primary objective was to elucidate the effect of the ITD on end tidal CO2, diastolic blood pressure, coronary perfusion pressure, and return of spontaneous circulation (ROSC). Their results not only showed that the usage of an ITD with active CPR improved end tidal CO2 and mean peak arterial pressures, but also 70% higher mean coronary perfusion when compared to the control group. They further demonstrated a decreased time to ROSC in the patients with the ITD. Although the utilization of ITDs with active CPR appear to have a benefit based on this study, only 21 patients were included decreasing the strength of this study. A second study was performed by Plaisance in 2004, but this time the objective looked at 24-hour survival in 400 patients [14]. This study was also a randomized controlled double-blinded prospective trial comparing active CPR with ITD to active CPR alone. They found a statistically significant increase number of patients surviving to 24 hours when ITD was used (64% in the ITD group compared to 44% when active CPR is used alone; OR 1.67 [1.07-2.6]) compared to the control.
The early successes of the Plaisance trials were echoed by the prospective controlled trial performed by Wolcke et al in 2003. Wolcke et al performed a prospective controlled trial comparing standard CPR to active CPR with ITD [15]. Their primary end point was 1-hour survival and 24-hour survival. They noted that nearly twice as many witnessed arrest patients survived for 1 hour and 24 hours when active CPR with ITD was used as compared to standard CPR alone (OR 2.4 [1.28-4.62]). However, a major critique of this study is that the authors compared standard CPR against two different variables, active CPR and ITD use, leading to serious confounding variables. This limitation is echoed in future studies. Other critiques include the size of the study (only 200 patients) and the lack of blinding.
These previous studies were the backbone for the 2005 AHA guidelines recommending the use of ITD in resuscitations, despite the fact no long-term survival benefit had been demonstrated [16]. In an attempt to address this perceived deficiency, a systematic review and meta-analysis was performed by Cabrini et al in 2008. This analysis looked at 5 studies including 833 patients and found improved ROSC (46% for ITD compared to 36% control, relative risk 1.45 [1.16-1.80]) and early survival (32% in those with ITD use compared to 22% without, RR 2.35[1.30-4.24]) [17]. They did not find a benefit in survival at the longest available follow-up or in favorable neurologic outcome when looking at all survivors.
In an effort to find a difference between long-term survival and overall neurological outcome, a multi-center, randomized-controlled, blinded, prospective study was completed by Aufderheide et al. Over 1,600 patients from 7 different locations and 46 EMS agencies in the United States were selected with the exception of patients believed to have an arrest from non-cardiac causes [18]. They compared standard CPR to active CPR with ITD and found improvement in survival to hospital discharge with favorable neurological function when active CPR with ITD was used (6% in standard CPR compared to 9% in the active CPR with ITD [OR1.58; 1.07-2.36]). Additionally, a 1-year survival was improved when active CPR with ITD was used compared to standard CPR alone (9% vs 6%; p=0.03). A follow up study looking at all patients, from both cardiac and non-cardiac causes, found that while standard CPR and active CPR with ITD had similar rates of ROSC, the active CPR with ITD had a 38% increase survival to discharge with favorable neurological outcome (OR 1.42 [CI 1.04-1.95]) and a 39% relative increase in survival to 1 year. These studies were widely criticized for using the ITD in active CPR and comparing the results to standard CPR alone. The benefit of survival could not be attributed to the ITD alone, as active CPR may have been part (or all) of the benefit. Hmmm…

In response to criticisms, Aufderheide et al. performed the largest randomized, double blinded, prospective study comparing standard CPR with standard CPR with ITD with the objective of assessing survival to hospital discharge with a favorable neurological outcome (modified Rankin score of 3 or less), known as the ROC PRIMED trial [19]. The study included 10 sites across the US and Canada involving 8,718 patients. Surprisingly, this study showed no difference in survival to hospital discharge with favorable neurological outcome (6.0% in the standard CPR with sham ITD compared to 5.8% in the standard CPR with active ITD). To further support the findings in the NIH PRIMED trial a subsequent systematic review and meta-analysis was performed that showed no survival benefit [20]. The authors noted significant heterogeneity between studies and that the ROC PRIMED study was by far the largest, significantly weighing results. However, a sub-analysis looking at the use of ITD in active CPR found potential benefit. The authors noted an increased likelihood of ROSC (odds ratio=1.19 [1.00-1.40], p=0.045), favorable neurologic outcome (odds ratio=1.60 [1.14-2.25]), and long-term survival (odds ratio=1.52 [1.11-2.08]) in those patients resuscitated with an ITD. These findings are reflected in the newest AHA guidelines in which it states that “[t]he routine set of ITD as an adjunct during conventional CPR is not recommended. The combination of ITD with active compression decompression CPR may be a reasonable alternative to conventional CPR in settings with available equipment and properly trained personnel [Class III recommendation].” [21]
Despite the newest AHA recommendations, the discussion on the potential benefit of the ITD is far from over. Yannopoulos et al re-evaluated the data collected in the ROC PRIMED trial to evaluate the quality of CPR performed during the study [22]. They found that of the 8,719 patients in the study, only 1,675 had quality CPR recorded. Of those who received acceptable CPR, ITD use with standard CPR increased survival to hospital discharge with modified Rankin score equal or less than 3 (7.2% compared to 4.1%; p=0.007). However, when the quality of CPR was not acceptable, the group receiving standard CPR with the ITD had a worse survival to hospital discharge with good neurological outcome (3.4% compared to 5.8%; p=0.007).
The complex interplay between multiple factors was again supported by the most recent systematic review and meta-analysis performed by Wang et al [23]. This meta-analysis looked at 15 studies to evaluate if either active CPR or ITD showed benefit over standard CPR. They compared active to standard CPR, standard CPR to standard CPR with ITD, and standard CPR to active CPR with ITD. They found no benefit for ITD or active CPR. However, in a regression analysis they found the results of their analysis may have been mitigated by the confounding variables of witnessed arrest and response time. When those two factors were adjusted, they found improved ROSC with ITD and active CPR. The meta-analysis again noted heterogeneity between studies, but stated that the biggest effect on survival was actually witnessed arrest and response times.
Take Home Points
Although initial studies demonstrated great potential for the ITD, the current, more powered studies do not absolutely support the use of the ITD with standard CPR. The limited benefit of the ITD may be confounded by other factors affecting CPR, such as the depth and rate of chest compressions. Future studies may show a benefit for the ITD in quality CPR. There is a potential benefit for the use of the ITD in active CPR, but this benefit is questionable. It is also difficult to state that any survival benefit is from the ITD and not the active CPR. What can be said is that early, good chest compressions and CPR does in fact show benefit. Once an EMS system masters these crucial initial steps, then perhaps devices like the ITD and processes like active CPR can provide a meaningful outcome for your patients.

References
1) Mozzaffarian D, Benjamin E, Go A. Heart Disease and Stroke Statistics-2015 Update. Circulation. 2015; 206-209.
2) Andreka P, Frenneaux M. Haemodynamics of cardiac arrest and resuscitation. Curr Opin Crit Care. 2006; 12:198-203.
3) Yannopolous D, Aufderheide T, Abella B, et al. Quality of CPR: An important effect modifier in cardiac arrest clinical outcomes and intervention effectiveness trials. Resuscitation. 2015; 94:106-113,
4) Aufderheide TP, Alexander C, Lick C, et al. From laboratory science to six emergency medical services systems: New understanding of the physiology of cardiopulmonary resuscitation increases survival rates after cardiac arrest. Brit Care Med October 2008;36(11)[Suppl.]S397-S404.
5) Schleien S, Berkowitz I, Trastman R, Rogers M. Controversial Issues in Cardiopulmonary Resuscitation. Anesthesiology. 1989; 71:133-149.
6) Jude W. Kouwenhoven W, Ing, Knickerbocker G. Cardiac Arrest. 1961; 178(11): 85-92.
7) Rudikoff M. Maughan L, Effron M, Freund P, Weisfeldt M. Mechanisms of Blood Flow During Cardiopulmonary Resuscitation. Circulation. 1980; 61(2):345-352. doi: 10.1161/01.CIR.61.2.345.
8) Lurie K, Coffeen P, Shultz J, McKnite S, Detloff B, Mulligan K. Improving Active Compression-Decompression Cardiopulmonary Resuscitation with an Inspiratory Impedance Valve. 1995;91:1629-1632. doi:10.1161/01.CIR.91.6.1629
9) Mader T, Kellogg A, Smith J, Decoteau R, et.al. A blinded, randomized controlled evaluation of an impedance threshold device during cardiopulmonary resuscitation in swine. Resuscitation 2008; 77:387-394.
10) Menegazzi JJ, Salcido DD, Menegazzi MT, et al. Effects of an impedance threshold device on hemodynamics and restoration of spontaneous circulation in prolonged porcine ventricular fibrillation. Prehosp Emerg Care. 2007; 11(2):179-85.
11) Shih A, Udassi S, Porvasnik S, et al. Use of Impedance threshold device in conjunction with our novel adhesive gloe device for ACD-CPR does not result in additional chest decompression. Resuscitation. 2013; 84:1433-1438.
12) Plaisance P, Lurie K, Payen D. Inspiratory Impedance During Active Compression-Decompression Cardiopulmonary Resuscitation: A Randomized Evaluation in Patients in Cardiac Arrest. Circulation. 2000; 101;989-994.
13) Plaisance P, Lurie K, Vicaut E et al. Evaluation of an impedance threshold device in patients receiving active compression-decompression cardiopulmonary resuscitation for out of hospital cardiac arrest. Resuscitation. 2004; 61:265-271.
14) Wolcke B, Mauer D, Schoefmann M et al. Comparison of Standard Cardiopulmonary Resuscitation Versus the Combination of Active Compression-Decompression Cardiopulmonary Resuscitation and an Inspiratory Impedance Threshold Device for Out-of-Hospital Cardiac Arrest. Circulation. 2003; 108;2201-2205.
15) AHA guidelines 2005
16) Cabrini L, Beccaria P, Landoni G et al. Impact of impedance threshold devices on cardiopulmonary resuscitation: A systematic review and meta-analysis of randomized controlled studies. Crit Care Med. 2008; 35(5);1625-1632. DOI: 10.1097/CCM.0b013e318170ba80.
17) Aufderheide T, Frascone R, Wayne M, et al. Standard cardiopulmonary resuscitation versus active compression-decompression cardiopulmonary resuscitatin with augmentation of negative intrathoracic pressure for out-of-hospital cardiac arrest: a randomized trial. Lancet. 2011; 377:301-311. DOI:10.1016/S01406736(10)62103-4.
18) Aufderheide T, Nichol G, Rea T et al. A Trial of an Impedance Threshold Device in Out-of-Hospital Cardiac Arrest. N Engl J Med 2011; 365:798-806.
19) Biondi G, Abbate A, Landoni G, Zangrillo A, Vincent J, D’Ascenzo F, Frati G. An updated systematic review and meta-analysis on impedance threshold devices in patients undergoing cardiopulmonary resuscitation. Heart, Lung and Vessels. 2014; 6(2): 105-113.
20) AHA 2015 guidelines
21) Yannopolous D, Aufderheide T, Abella B, et al. Quality of CPR: An important effect modifier in cardiac arrest clinical outcomes and intervention effectiveness trials. Resuscitation. 2015; 94:106-113.
22) Wang C, Tsai M, Chang W, et al. Active Compression-Decompression Resuscitation and Impedance Threshold Device for Out-of-Hospital Cardiac Arrest: A Systematic Review and Metaanalysis of Randomized Controlled Trials. Crit Care Med. 2015; 43(4):889-896. DOI: 10.1097/CCM.0000000000000820.
Images from:
https://media.giphy.com/media/eeOCVjeNd6oxy/giphy.gif
http://sd.keepcalm-o-matic.co.uk/i/keep-calm-and-stick-to-the-basics.png
https://rmarks6.files.wordpress.com/2014/12/react.gif