On December 5th we posted the following case for discussion and asked our readers to comment on the management of refractory ventricular fibrillation. Here is the summary of comments received, both on the blog, and via twitter.
The Case….
A 56 year-old male is cleaning out his garage with his wife when she hears him fall. She turns around to find him unresponsive on the ground. He is making gasping breath sounds but otherwise does not respond when she shakes him and yells at him. She is instructed to perform CPR by pre-arrival instructions after calling 911 on her cellphone. Within minutes, the BLS Fire Department arrives and takes over. After confirming that the patient is pulseless, they resume CPR while applying an AED. The AED states “shock advised” for ventricular fibrillation. After resuming CPR after one shock is delivered, the ALS ambulance arrives. High performance CPR is continued and the patient is defibrillated three more times for persistent ventricular fibrillation. The end-tidal CO2 is 40 mmHg. The patient has now been pulseless for almost twenty minutes. The paramedics plan on continuing high performance CPR, but wonder what they will do if the patient remains in ventricular fibrillation with a good end-tidal 10 minutes from now…
Improvements in the care of patients with out-of-hospital cardiac arrest have changed patient outcomes dramatically. More uniform collection of out-of-hospital cardiac arrest data has allowed benchmarking and the identification of high performance CPR as the key ingredient in neurologically intact survival. We have learned that doing the basics well makes the critical difference. Cardiac arrest management has undergone a major transition from the ‘load and go’ strategy to high-performance CPR on scene.
However, a small proportion of out-of-hospital cardiac arrest patients may benefit from more than what we typically are able to offer prehospital. Emerging evidence suggests that patients with refractory ventricular fibrillation(VF) may be one such population. However, as pointed out by comments made by Dr. Aurora Lybeck, this population remains ill-defined:
“One major issue/barrier to researching this in a meaningful way is that there doesn\’t seem to be a consensus definition of what “refractory” or “persistent” VF/pVT is. Is it 3 shocks? 5? 7? a predefined number of minutes? To date, there doesn\’t seem to be even a majority agreement as to how we define this.” – Aurora Lybeck
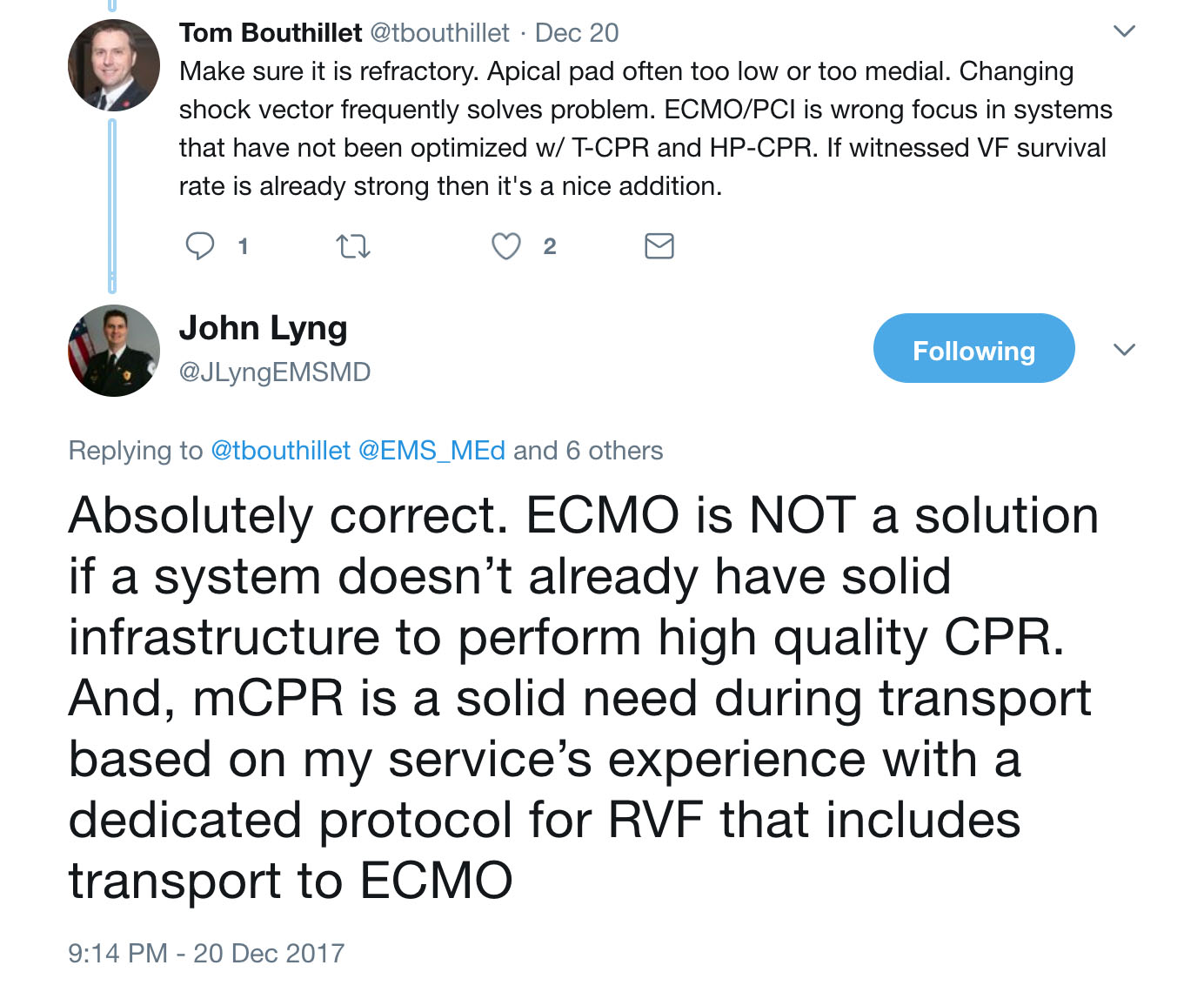
One Japanese study defined refractory ventricular fibrillation as presentation to the hospital in ventricular fibrillation after at least one out-of-hospital defibrillation [1]. In this study, refractory VF accounted for 23% of all patients with VF as a presenting rhythm and 4% of witnessed OHCA. In other studies, refractory VF was VF that was unresponsive to at least 3 defibrillation attempts and administration of 300 mg of IV amiodarone [2], or a median of 6 defibrillation attempts and anti-arrhythmic administration [3]. As discussed over twitter by Tom Bouthillet and John Lyng, “refractory” may be considered persistent VF despite already excellent high-performance CPR and correctly performed defibrillation:
If at minimum we define refractory VF as VF unresponsive to the best we have to offer with standard high performance prehospital ALS care, what are some of the non-standard interventions that we may be able to offer?
“There is an ever- growing body of literature to help us understand at least how to get the patient OUT of VF/VT. We are better understanding therapeutic options, be it pharmaceutical, electric (shameless plug for changing pad vectors, double sequential defibrillation), or some of the more aggressive options such as ECMO, an amazing but obviously not universally feasible option” – Aurora Lybeck
Dr. Lybeck starts by mentioning pharmaceutical options and double sequential defibrillation. Let’s review the evidence regarding these as adjuncts to high performance CPR.
Pharmaceutical options: Recently, a small number of observational studies have been published suggesting that esmolol administration should be considered for patients in refractory ventricular fibrillation. In a paper published in 2014, Driver et. al. reviewed the cases of 25 patients with OHCA and refractory ventricular fibrillation (no ROSC despite three defibrillation attempts, 300 mg of amiodarone and 3 mg of epinephrine) and arrival in ED with persistent ventricular fibrillation [3]. They compared patients with received esmolol (n=6) to patients who did not (n=19). Patient’s had a similar proportion of patients with VF as their presenting rhythm and with witnessed arrest. 3/6 (50%) of patients receiving esmolol survived to hospital discharge with good neurologic outcome compared with 2/19 (10.5%) of patients in the no-esmolol group. A subsequent paper published in 2016 by a Korean group (Lee et. al.) was a pre-post study of inclusion of esmolol in a treatment algorithm for refractory VF [4]. Using the same inclusion criteria as the Driver et. al. study, they compared patients who did and did not receive esmolol. While patients who received esmolol were more likely to get ROSC [9/16 (53%) vs. 4/25 (16%)], there was no statistically significant difference in neurologically-intact survival at 30 days (18.8% in esmolol group vs. 8% in non-esmolol group). The numbers were overall very small.
Double Sequential Defibrillation: Double Sequential defibrillation (DSD), the use of two sets of pads and defibrillators to deliver two nearly simultaneously shocks at two different vectors, has gained attention as a therapy for refractory ventricular fibrillation. The majority of examples are case reports [5] or case series [6]. The few retrospective studies that have been published have very small numbers of patients who received the therapy. In Ohio, a retrospective study of 2428 patients with OHCA found that 12 were treated with DSD. Of these, 9 patients were converted out of VF, with 2 surviving to hospital discharge with a good neurologic outcome (CPC 1 or 2) [7]. A subsequent retrospective review of DSD use in OHCA in London found that of 45 patients treated with DSD in an 18 month period, only 7% survived to hospital discharge. This rate was comparable to a that in a comparator group that continued to receive standard defibrillation alone [8]. The jury on double sequential defibrillation is still undecided and a randomized control trial does not exist, but it remains something to consider in the case of refractory VF.
Above and beyond drugs and electricity, Dr. Lybeck mentions another less available but more aggressive intervention – ECMO (aka ECPR). The goal of ECMO is to restore oxygenation and perfusion while enabling interventions that treat the underlying etiology of the arrest. In the case of refractory VF, it is worthwhile thinking about etiologies that are not reversible with standard prehospital ALS care. The most common etiology for refractory Vfib in multiple studies is acute coronary syndrome, anywhere from 42.1% in a French study to 84% in a study in Minnesota [2,8]. Other less common etiologies include aortic dissection and pulmonary embolism [3]. This suggests that what a subset of patients with refractory VF need is coronary reperfusion therapy in order to re-establish a perfusing rhythm.
ECMO/ Extracorporeal Life Support (ECLS) and coronary reperfusion therapy has been pursued in a number of EMS systems internationally, some with very impressive results. The CHEER trial was carried out in Melbourne, Australia [10]. They utilized a combination of mechanical CPR, hypothermia, ECMO and early reperfusion for patients with refractory cardiac arrest. Inclusion criteria included age 18-65 years, cardiac arrest due to suspected cardiac etiology, chest compressions initiated within 10 minutes by bystanders or EMS, an initial rhythm of VF and availability of mechanical CPR. A total of 11 patients were transported over a 32 month period and 9 received ECLS. Five of 11 (45%) transported patients survived with good neurologic outcome. Subsequently, a larger trial has been carried out in the United States (Minnesota). Using a more protocolized approach, patients with VF/VT as their initial rhythm, age 18-75 yrs and VF refractory to 3 EMS delivered shocks, 300 mg of IV/IO amiodarone, lack of pre-existing severe comorbidities or terminal illness, body habitus to fit within a mechanical CPR device and estimated transfer time from scene to the cardiac catheterization lab < 30 minutes were transported with mechanical CPR in progress. ECLS was initiated in the cardiac catheterization lab and patients underwent cardiac catheterization which identified coronary occlusion in 84%. 62 patients met transport criteria and 55 had ECLS initiated. Of these, 28 (45%) survived to hospital discharge, 26 of whom (42%) had good neurologic outcome [2]. This was better than outcomes in a historical comparison group (15.3% neuro-intact survival). These findings are consistent with a prior prospective observational study in Japan comparing outcomes for patients with refractory VF who underwent conventional cardiopulmonary resuscitation versus ECLS [11]. The authors compared neurologically-intact survival for patients transported to tertiary centers that performed ECLS on standard protocol versus those that did not. They found that patients who received ECLS had significantly high neurologically-intact survival (12.3%) than those who did not (1.5%), although these rates were overall lower than those documented in the CHEER and Minnesota trials. This trial was unable to account for differences in baseline care between ECLS and non-ECLS tertiary care centers.
ECLS, however, is a resource-intensive endeavor. Low threshold for implementation of advanced therapies such as EPCR is not likely to lead to a high value intervention. Can we identify patients who both require advanced therapies to convert out ventricular fibrillation and are likely to do well?
With the respect to our case, In Princess Bride-like form, Dr. Jeremiah Escajeda stated the following: “This patient has aliveness. He should be transported …”

What features of this patient’s case make it so that he is only “mostly dead”? Dr. Escajeda goes on to share the criteria in the Pittsburgh area for transport for EPCR:
“We have a prehospital alert system in place here in Pittsburgh that when providers identify a refractory organized rhythm, in a “young,” healthy person, they speak with a command physician to run our prehospital ECPR checklist. If criteria are met, the patient is then expeditiously transported to our ECPR center with an alert sent to our ECMO team, ED team, Post Cardiac Arrest team and Cardiology. After the patient is placed on the circuit, next destination is cath lab.
Here is the prehospital checklist:
* Strongly suggested to place patient on LUCAS Device as soon as available
* Call attending medic command physician to run checklist
[ ] Witnessed arrest
[ ] Bystander CPR
[ ] Age ≥ 18 and ≤60
[ ] Initial shockable rhythm or PEA rate > 20 bpm
[ ] Good functional status prior to arrest (patient living independently and not from a skilled nursing facility/ LTAC and no prior neurocognitive dysfunction)
[ ] No signs of irreversible organ dysfunction (such as COPD on home O2, stigmata of liver cirrhosis or ESRD such as AV fistula or terminal cancer)
[ ] No morbid obesity (Morbid obesity defined as inability to fit into LUCAS device and/or abdominal pannus overhanging inguinal crease)
[ ] End tidal CO2 >10 mmHg with CPR
[ ] Expected time from collapse to ED arrival <= 30 mins
Hey maybe even one day we will be placing ECLS devices prehospital, has this has already been done in France https://www.ncbi.nlm.nih.gov/pubmed/28414164
and now they have impella devices that deliver 5L/min, and are the size of a pencil. Exciting future for these refractory cases.”

Image Source/Reference: Reynolds, J. C., Grunau, B. E., Elmer, J., Rittenberger, J. C., Sawyer, K. N., Kurz, M. C., … & Callaway, C. W. (2017). Prevalence, natural history, and time-dependent outcomes of a multi-center North American cohort of out-of-hospital cardiac arrest extracorporeal CPR candidates. Resuscitation.
This prehospital checklist accounts for factors that we already know are associated with favorable neurologically-intact survival from OHCA. But a critical question (and perhaps gets back to the question of the term “refractory”) is at what time interval should we start thinking about transporting the patient? How can we identify patients who have received the maximum potential benefit of on-scene care while still retaining benefit from care escalation in the form of ECLS? Many patients will achieve ROSC without EPCR and initiating EPCR too early may distract from continuous, high-quality chest compressions. The Pittsburgh protocol of time of collapse to ED arrival of < 30 minutes has evidence behind it. A retrospective study of patients with OHCA within the ROC consortium examined the probability of good neurologic outcome in patients who would be considered eligible for EPCR (met age and pre-cardiac arrest functional status data) versus duration of resuscitation [12]. They found that amongst all eligible patients, the probability of neurologically-intact survival dropped below 10% after 30 minutes of resuscitation (see Figure). They thus concluded that mobilization towards EPCR resources should be considered after 9-20 minutes of active resuscitation. Interestingly, amongst patients who achieved ROSC, longer durations of CPR were no longer associated with impaired neurologic outcomes (See Figure). The results of this study concurred with a prior study of consecutive patients age < 65 with witnessed arrest and initiation of CPR in < 10 minutes that concluded that “transport for ECPR should be considered between 8 to 24 minutes of professional on-scene resuscitation, with 16 minutes balancing the risks and benefits of early and later transport. Earlier transport within this window may be preferred if high quality CPR can be maintained during transport and for those with initial non-shockable rhythms.” [13]
Conclusion
In the end, every EMS system has a limited amount of time and resources for training. The healthcare system itself is resource-limited. After years of focus on “Airway” before “Circulation”, we have come to the understanding that we need to focus on circulation; excellent BLS care in the form of high quality CPR and early defibrillation is the cornerstone of cardiac arrest care. However, there are a subset of patients with potential for neurologically-intact survival that may be saved by additional circulatory intervention, including extracorporeal support and coronary reperfusion therapy. Identifying who these patients are and the best way to both provide this therapy while utilizing limited healthcare resources in a high value manner may be the future of cardiac arrest care.
Dr. Lybeck said it best, so we’ll end with her quote:
“Particularly on the topic of OHCA, it\’s an exciting time to be an EMS physician, many thanks to our researchers, educators, and advocates out there, keep up the great work!”
Case Summary by Maia Dorsett, MD PhD, @maiadorsett
References:
1. Sakai, T., Iwami, T., Tasaki, O., Kawamura, T., Hayashi, Y., Rinka, H., … & Kajino, K. (2010). Incidence and outcomes of out-of-hospital cardiac arrest with shock-resistant ventricular fibrillation: data from a large population-based cohort. Resuscitation, 81(8), 956-961.
2. Yannopoulos, D., Bartos, J. A., Raveendran, G., Conterato, M., Frascone, R. J., Trembley, A., … & Wilson, R. F. (2017). Coronary artery disease in patients with out-of-Hospital refractory ventricular fibrillation cardiac arrest. Journal of the American College of Cardiology, 70(9), 1109-1117.
3. Driver, B. E., Debaty, G., Plummer, D. W., & Smith, S. W. (2014). Use of esmolol after failure of standard cardiopulmonary resuscitation to treat patients with refractory ventricular fibrillation. Resuscitation, 85(10), 1337-1341.
4. Lee, Y. H., Lee, K. J., Min, Y. H., Ahn, H. C., Sohn, Y. D., Lee, W. W., … & Park, S. O. (2016). Refractory ventricular fibrillation treated with esmolol. Resuscitation, 107, 150-155.
5. Lybeck, A. M., Moy, H. P., & Tan, D. K. (2015). Double sequential defibrillation for refractory ventricular fibrillation: a case report. Prehospital emergency care, 19(4), 554-557.
6. Cabañas, J. G., Myers, J. B., Williams, J. G., De Maio, V. J., & Bachman, M. W. (2015). Double sequential external defibrillation in out-of-hospital refractory ventricular fibrillation: a report of ten cases. Prehospital emergency care, 19(1), 126-130.
7. Cortez, E., Krebs, W., Davis, J., Keseg, D. P., & Panchal, A. R. (2016). Use of double sequential external defibrillation for refractory ventricular fibrillation during out-of-hospital cardiac arrest. Resuscitation, 108, 82-86.
8. Emmerson, A. C., Whitbread, M., & Fothergill, R. T. (2017). Double sequential defibrillation therapy for out-of-hospital cardiac arrests: the London experience. Resuscitation.
9. Pozzi, M., Koffel, C., Armoiry, X., Pavlakovic, I., Neidecker, J., Prieur, C., … & Obadia, J. F. (2016). Extracorporeal life support for refractory out-of-hospital cardiac arrest: should we still fight for? A single-centre, 5-year experience. International journal of cardiology, 204, 70-76.
10. Stub, D., Bernard, S., Pellegrino, V., Smith, K., Walker, T., Sheldrake, J., … & Cameron, P. (2015). Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation, 86, 88-94.
11. Sakamoto, T., Morimura, N., Nagao, K., Asai, Y., Yokota, H., Nara, S., … & SAVE-J Study Group. (2014). Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: a prospective observational study. Resuscitation, 85(6), 762-768.
12. Reynolds, J. C., Grunau, B. E., Elmer, J., Rittenberger, J. C., Sawyer, K. N., Kurz, M. C., … & Callaway, C. W. (2017). Prevalence, natural history, and time-dependent outcomes of a multi-center North American cohort of out-of-hospital cardiac arrest extracorporeal CPR candidates. Resuscitation.
13. Grunau, B., Reynolds, J., Scheuermeyer, F., Stenstom, R., Stub, D., Pennington, S., … & Christenson, J. (2016). Relationship between time-to-ROSC and survival in out-of-hospital cardiac arrest ECPR candidates: When is the best time to consider transport to hospital?. Prehospital Emergency Care, 20(5), 615-622.