The Article:
Wang HE, Schmicker RH, et al. (2018). Effect of a Strategy of Initial Laryngeal Tube Insertion vs Endotracheal Intubation on 72-Hour Survival in Adults With Out-of-Hospital Cardiac Arrest. JAMA, 320(8), 769.
Background & Objectives:
Airway management has long been one of the first steps in the ABC’s of cardiac arrest management, but there has recently been growing evidence that early definitive airway management may not necessarily lead to improvement of meaningful outcomes. In 2018, there were 3 landmark papers published in JAMA that attempted to shed light on which method of airway management was better in out-of-hospital cardiac arrest (OOHCA).
-
Trial 1 – BVM vs ETI, where use of BVM compared with ETI failed to demonstrate noninferiority or inferiority for survival with favorable 28-day neurological function. [1]
-
Trial 2 – i-Gel SGA vs ETI (AIRWAYS-2), where randomization to a strategy of advanced airway management with a supraglottic airway compared with tracheal intubation did not result in a favorable functional outcome at 30 days. [2] (See Article Bite #14 for more in-depth discussion of this trial: http://www.naemsp-blog.com/emsmed/2019/9/14/article-bites-14-to-tube-or-not-to-tube-in-cardiac-arrest)
So, we essentially have a scientific “tie” between BVM vs ETI and i-Gel vs ETI with respect to their primary outcomes studied (although I strongly suggest you read the secondary outcomes and decide for yourself). However, like in sports and politics, we attempt to declare a winner in the end, and the question about which method of airway management is best cannot be left in this state of uncertainty.
Enter the third published trial of 2018, where Henry Wang et al sought to determine the effect of King-LT vs endotracheal intubation on 72-hour survival in adult OOHCA.
Methods:
This was a multicenter, pragmatic, cluster-crossover, open-label, randomized trial involving 27 EMS agencies across the US in 13 clusters, with clusters crossing over at 3-5 month intervals.
-
Patients: Adults (18+) with non-traumatic OOHCA requiring ventilatory support or advanced airway management
-
Intervention: Initial airway management with King-LT
-
Comparison: Initial endotracheal intubation (ETI)
-
Protocol allowed for use of paralytics and video laryngoscopy
-
Protocol allowed for airway rescue attempt with any technique if the initial attempt was unsuccessful, but did not limit the number of attempts
-
-
Outcome
-
Primary: 72-hour survival
-
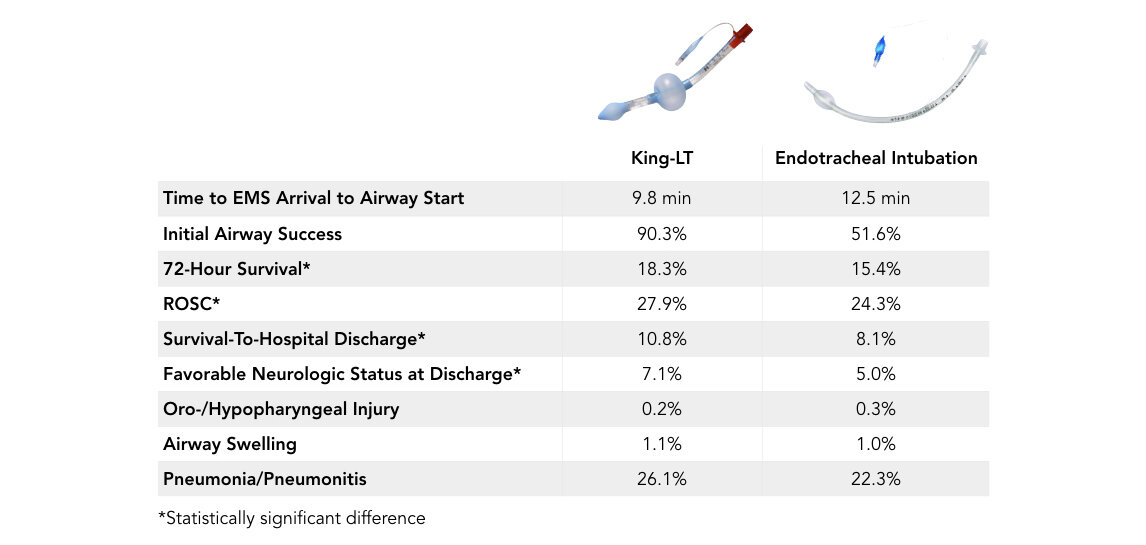
Secondary: ROSC, survival-to-hospital discharge, favorable neurologic status at hospital discharge (mRS </= 3), and key adverse events
-
Key Results:
-
3004 enrolled patients between December 1, 2015 and November 4, 2017
-
Initial King-LT – 1,505 patients
-
Initial ETI – 1,499 patients
-
Takeaways:
This trial demonstrated that the King-LT is faster to attempted airway placement (by an average of 2.7 minutes) and required fewer insertion attempts for successful airway placement, which could have implications in improved CPR quality and thus the improved primary and secondary outcomes, although this trial did not measure CPR quality specifically.
Furthermore, this trial did demonstrate statistically significant differences in 72-hour survival, ROSC, survival-to-hospital discharge, and favorable neurologic status at discharge with the King-LT compared to endotracheal intubation.
The initial ETI success rate of 51.6% is much lower than previously published studies, and could be multi-factorial. A primary reason could be that many EMS medical directors encourage earlier use of the supraglottic airway to avoid multiple intubation attempts, in order to avoid chest compression interruptions.
What This Means For EMS:
On the surface, it seems that we finally have a “winner”, that the King-LT leads to improved meaningful outcomes compared to endotracheal intubation in adult OOHCA. However, on further examination, it seems that we are comparing this supraglottic device to a strategy which utilizes inferior endotracheal intubation skills, given the ETI first-pass success rate of 51.6%, with 20% of patients requiring 3 or more airway attempts.
We cannot assume that this low success rate was due to inadequate training, although that may have been the case. As many of us with EMS backgrounds know, it could be due to the complexity of the environment, the acuity of the patients, or a lack of experience.
Even if we made the assumption that the first-pass ETI success rate would improve with increased training, and spent a ton of time and money training and buying fancy equipment and improve our first-pass ETI success, AIRWAYS-2 showed us that there was no difference in favorable neurologic outcomes at 30 days with i-Gel (87.4% success rate) vs ETI (70% success rate). Ultimately, we would spend a lot of time, money, and energy to achieve a “no difference” between the strategies.
Even in the Jabre study, they had physicians working in EMS systems who were very skilled in intubation, and there was still no significant difference in their intubation vs use of a simple BVM in 28-day neurologic outcome.
Some might argue that the reason for improved primary and secondary outcomes with the King-LT is because the CPR quality was probably higher, since you could easily deduce that the airway was faster and easier to place, and with fewer attempts overall. However, we must be careful because this study did not specifically measure this.
What the accumulated studies are showing us is that the management of the airway during cardiac arrest is of minimal clinical consequence, and can often become a distraction from the things that would improve survival in cardiac arrest, such as emphasis on high-quality CPR and early defibrillation…you know, the basics.
Recognizing that intubation is becoming a high-risk, low-frequency prehospital skill that is expensive and complex to maintain proficiency, these recent studies do not support the costs of maintaining this skill.
Perhaps it is time to do a randomized controlled trial comparing nasal cannula with a jaw thrust, BVM with capnography, i-Gel, King-LT, and endotracheal intubation, and maybe we can finally put this argument to rest?
Ultimately, when you are working your next adult OOHCA, you should employ the airway strategy for which you are most efficient, or which is the simplest and fastest, limiting distractions and interruptions in CPR, focusing on the basics and fundamentals, which likely are the interventions that truly matter in achieving those meaningful patient outcomes.
References:
1. Jabre P, Penaloza A, et al. (2018). Effect of Bag-Mask Ventilation vs Endotracheal Intubation During Cardiopulmonary Resuscitation on Neurological Outcome After Out-of-Hospital Cardiorespiratory Arrest. Jama, 319(8), 779. doi: 10.1001/jama.2018.0156
2. Benger JR, Kirby K, et al. (2018). Effect of a Strategy of a Supraglottic Airway Device vs Tracheal Intubation During Out-of-Hospital Cardiac Arrest on Functional Outcome. Jama, 320(8), 779. doi: 10.1001/jama.2018.11597
Article Bites Summary by: Brandon Morshedi, MD, DPT (@bbmorshedi)


