Article: Patterson PD, Higgins JS, Van Dongen HPA, Buysse DJ, Thackery RW, Kupas DF, et al. Evidence-based guidelines for fatigue risk management in emergency medical services. Prehosp Emerg Care 2018 Feb;22(sup1):89-101.
Background:
There is not a large amount of evidence in the EMS literature that guides how to mitigate workplace fatigue, which affects over half of all EMS personnel. Fatigue has been linked to injury of personnel and patients, errors in patient care, and adverse events. The shift work of EMS has also been shown (in other groups) to disrupt sleep patterns and contribute to fatigue. There are no guidelines for fatigue risk management in EMS, unlike in other high risk industries (rail, aviation, nuclear power); however, they are not based on evidence-based-guidelines. The goal of this investigation was to create and evidence-based guideline for fatigue management tailored to EMS operations.
Methods:
A systemic search was performed based on seven research questions from a Population, Intervention, Comparison, and Outcome (PICO) framework. Investigators included literature that was specific for EMS personnel or similar shift workers. The panel that was brought together reviewed summaries based on the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. Recommendations were then made based on the evidence and the Content Validity Index (CVI) was used to quantify the panels\’ agreement on each recommendation (for clarity and relevance). The panel consisted of experts in sleep medicine, fatigue science, emergency medicine, EMS, risk management, administration, and consumerism.
Key Results:
Question 1: Are there reliable and valid instruments for measuring fatigue among EMS personnel?
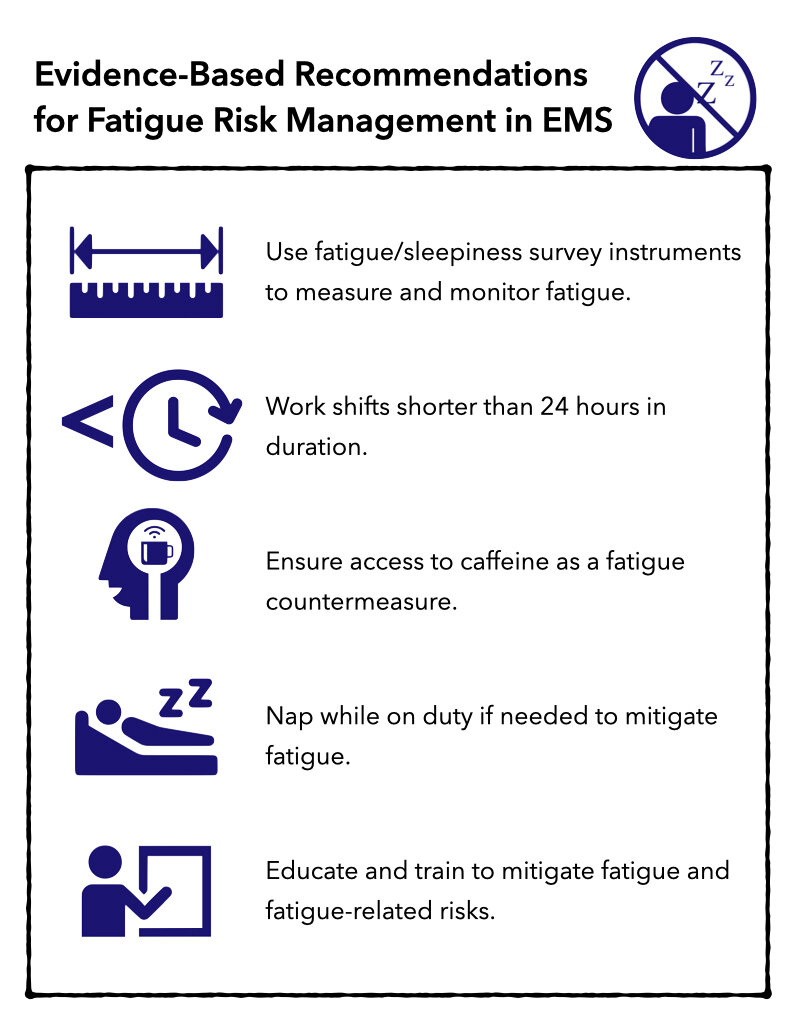
Recommendation 1: Recommend using fatigue/sleepiness survey instruments to measure and monitor fatigue in EMS personnel.
Strength of Recommendation: Strong
Quality of Evidence: Low
Remarks: Evidence was supportive for survey instruments, but none has undergone comprehensive reliability and validity measurements. There is no gold standard for assessment, so there were questions raised about the accuracy of surveys. Answers from surveys may be able to be used to leverage policies that limit work and invoke mandatory rest periods or personnel may answer questions to avoid lost opportunities for work/overtime.
Question 2: In EMS personnel, do shift-scheduling interventions mitigate fatigue, mitigate fatigue-related risks, and/or improve sleep?
Recommendation 1: Recommend that EMS personnel work shifts shorter than 24 hours in duration.
Strength of Recommendation: Weak
Quality of Evidence: Very Low
Remarks: Shifts less than 24 hours were found to be more favorable towards critical or important outcomes, but shorter shifts did not show a difference in comparison of 8 vs 12 hours (or other combinations). Shorter shifts were associated with reduced fatigue, improved alertness, better sleep and sleep quality, and increased safety but could cause higher costs to the system, reduced access to care for patients, and increased risks to personnel. This was found to be more important in rural/remote areas where personnel have to travel greater distances to work and the longer shifts may allow for additional employment due to less time spent traveling and transitioning to and from work.
Question 3: In EMS personnel, does the worker\’s use of fatigue countermeasures mitigate fatigue, mitigate fatigue-related risk, and/or improve sleep?
Recommendation 3: Recommend that EMS personnel have access to caffeine as a fatigue countermeasure.
Strength of Recommendation: Weak
Quality of Evidence: Low
Remarks: Evidence shows that there are positive effects of caffeine on psychomotor vigilance, but health and safety Issues such as anxiety and cardiac arrhythmias may cause negative symptoms. Also, long-term effects of caffeine use for fatigue mitigation is not well known.
Question 4: In EMS personnel, does the use of sleep or rest strategies and/or interventions mitigate fatigue, fatigue-related risk, and/or improve sleep?
Recommendation 4: Recommend that EMS personnel have the opportunity to nap while on duty to mitigate fatigue.
Strength of Recommendation: Weak
Quality of Evidence: Very Low
Remarks: The use of naps on shift is an effective strategy to positively impact fatigue-related outcomes and improve alertness and performance. However, sleep inertia (reduced alertness or impaired cognition) may occur immediately after wakening and the evidence did not address any optimal nap time. Naps <10 minutes decrease sleep inertia and naps 15-120 minutes area associated with better performance. No evidence was provided to demonstrate an impact on personnel safety.
Question 5: In EMS personnel, does fatigue training and education mitigate fatigue, fatigue-related risks, and/or improve sleep?
Recommendation 5: Recommend that EMS personnel receive education and training to mitigate fatigue and fatigue-related risks.
Strength of Recommendation: Weak
Quality of Evidence: Low
Remarks: A favorable relationship exists between education and training in fatigue and sleep health and important outcomes of patient and personnel safety, with improvements shown in 4-8 weeks after education and training. Some undiagnosed sleep disorders may be identified from this but costs of programs vary. However, they should be repeated with new orientation and every 2 years to prevent decay in knowledge and skills of fatigue mitigation.
Question 6: In EMS personnel, does implementation of model-based fatigue risk management mitigate fatigue, mitigate fatigue-related risks, and/or improve sleep?
Recommendation 6: No recommendation because of insufficient confidence in effect estimates.
Strength of Recommendation: Not applicable
Quality of Evidence: Very Low
Remarks: Findings from one study were favorable, but the body of evidence was insufficient to make a recommendation.
Question 7: In EMS personnel, do task load interventions mitigate fatigue, fatigue-related risk, and/or improve sleep?
Recommendation 7: No recommendation because of insufficient confidence in effect estimates.
Strength of Recommendation: Not applicable
Quality of Evidence: Very Low
Remarks: Definitions of task load and work load vary and none of the evidence reviewed investigated the relationship between work/task load and safety and cost.
Takeaways:
The panel does recommend using survey instruments for assessing and monitoring fatigue, scheduling shifts < 24 hours, providing caffeine during shifts, incorporating naps into on-duty time, and providing education in fatigue risk management.
What This Means for EMS:
There is no gold standard for mitigation of fatigue and fatigue-related risks in EMS, but with evidence-based guidelines, an initial set of recommendations can be made. However, these are going to have to take into account the type and location of EMS service and the ability to implement these recommendations before we can make broad ranging recommendations for all services.
Article Summary by Mark Levine, MD FAEMS



