Nightscales, R et al. “Mortality in Patients with Psychogenic Nonepileptic Seizures.” Neurology 95.6 (2020): e643–e652. Neurology.
Background
Caring for psychogenic nonepileptic seizure (PNES) patients (the condition formerly known as “pseudoseizures”) in the emergency setting can be exceedingly difficult and frustrating. This is understandable because discerning between true seizure activity and a psychogenic event leads to drastically different treatment pathways. Additionally, PNES patients have high rates of underlying substance use disorder and psychiatric illness which can further cloud the clinical picture. This is a difficult diagnosis for even the hospital neurologists demonstrated by the fact that PNES patient account for 25% of EEG unit admissions and a final diagnosis of PNES takes an average of eight years! If that’s not enough, between 5-20% of PNES patients also have true epilepsy. The objective of this study was to look at the disease progression and mortality characteristics of PNES patients.
Methods
This was a retrospective cohort study that included all admissions to three video EEG (the gold standard for epilepsy diagnosis) monitoring units in Victoria, Australia. Data from 1995 through 2015 was reviewed.
For diagnostic purposes, patients admitted for video EEG monitoring (VEM) were separated into three groups: PNES, epilepsy or the combination of the two. Then, chart review was linked to the Australian national death index (NDI) to correlate mortality rates and causes.
Key Results
There were 5,508 admissions to the VEM units during the study period. (674 with PNES, 3064 with Epilepsy, 75 with both and 1595 diagnosed as other). Brain tumor patients were excluded. The death rates over the 20-year study period for the three groups were as follows 8.2% PNES (55/674) 9.4% Epilepsy (288/3,064) and 8% Both (14/175).
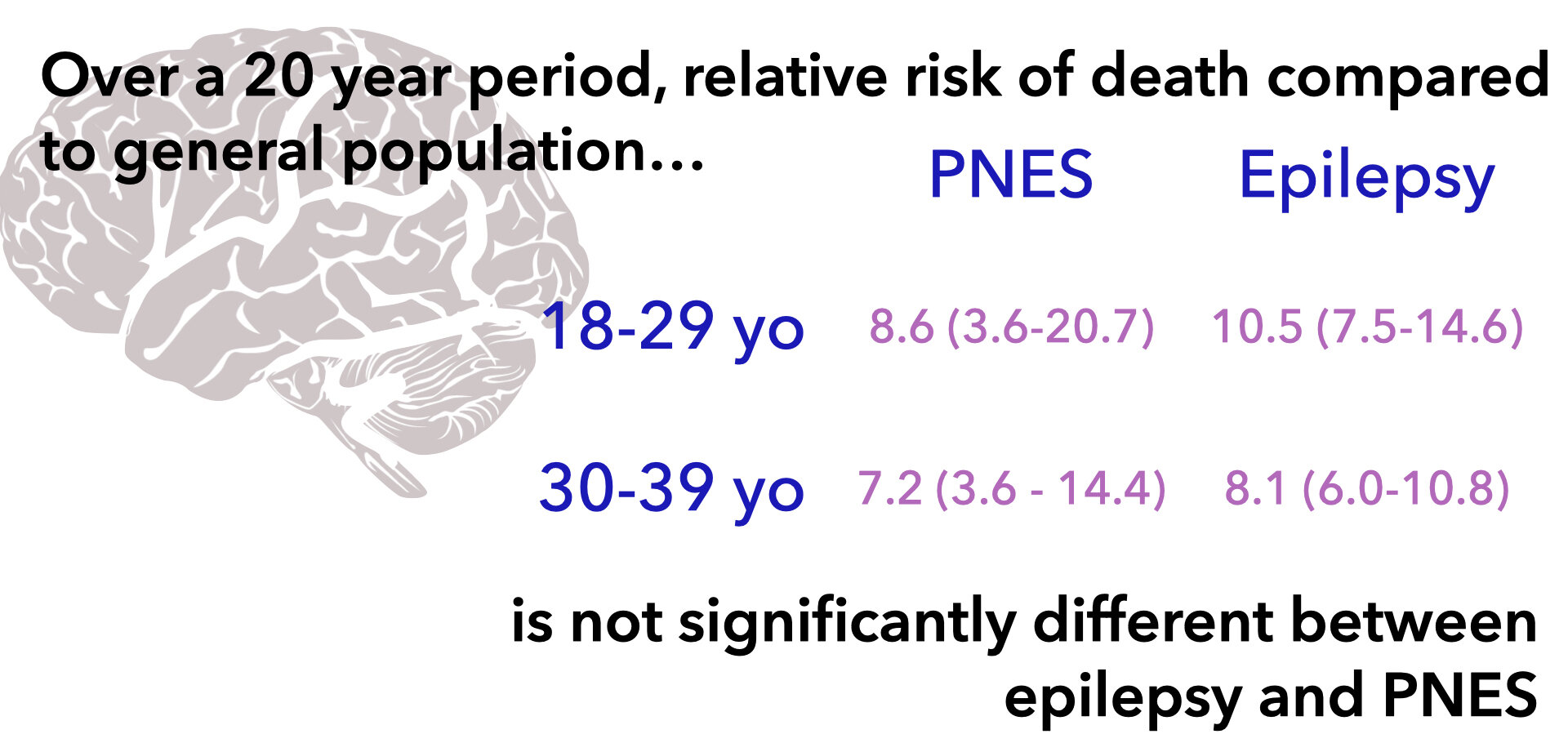
Compared to the standard population, the relative risk of death in PNES patients increased 8.8-fold in patients less than 30 years old. The authors saw NO significant difference in mortality between the epilepsy and PNES groups. Surprisingly, 24% of the PNES group had a cause of death listed as epilepsy. The authors then specifically reviewed those patient’s VEM results and found no hospital EEG findings to suggest epilepsy.
Another concerning finding was that ~20% PNES deaths were due to suicide or poisoning as compared to a 6.6% rate in the general population and an 11% rate in the epilepsy group. Also, PNES patients were more likely to live in the lowest socioeconomic areas.
What Else Do We Know About PNES?
There have been two prior PNES mortality studies. One from Scotland (n=260) that demonstrated an increased rate of premature death in PNES patients and another from Denmark (n=472) that showed a 3-fold increase in mortality in patients with PNES.
What Should We Do Now?
Be kind and empathetic, period – PNES is a “REAL” disease. Emergency providers must eliminate the idea that these patients are “fakers.” Patients with PNES are struggling both medically and socially with high rates of suicide, substance-use disorder and low socioeconomic status.
Also, beware of being too certain. 3% of VEM admits had diagnoses of both PNES and epilepsy and ~25% PNES deaths were due to “epilepsy.” Distinguishing between epilepsy and PNES can be impossible even for neurologists and the coroners.
The BOTTOM LINE…
PNES mortality is EQUAL to that of treatment resistant epilepsy. There is nothing “fake” or “pseudo” about that. We must treat these patients with kindness and empathy without passing judgment. This topic warrants much more discussion with additional research and work toward better treatment options in both the prehospital and hospital settings.
Article Bites Summary by Casey Patrick, MD (twitter @cpatrick_89)



