Article Summary by Casey Patrick, MD, FAEMS @cpatrick_89
Article: Pappal RD, Roberts BW, Mohr NM, Ablordeppey E, Wessman BT, Drewry AM, Winkler W, Yan Y, Kollef MH, Avidan MS, Fuller BM. The ED-AWARENESS Study: A Prospective, Observational Cohort Study of Awareness With Paralysis in Mechanically Ventilated Patients Admitted From the Emergency Department. Ann Emerg Med. 2021 Jan 20:S0196-0644(20)31314-7.
Background
On the list of “worst nightmares” is being paralyzed and awake, which is truly the stuff of horror movies. Anytime neuromuscular blockade medications are used in airway management, this phenomenon must be anticipated and prevented at all costs. There is a large volume of literature addressing and investigating the risks and incidence of paralysis while awake in the operating room setting. Surprisingly, however, there is a sparsity of emergency department (ED) research in this area. Many EMS systems allow the use of neuromuscular blockade in addition to sedation medications, making it incumbent for prehospital providers to have a solid pharmacologic and physiologic knowledge of the agents used to facilitate intubation.
This study’s goal was to quantify the rate of being awake and paralyzed following intubation in the ED and additionally attempted to investigate possible risk factors influencing its occurrence.
Methods
This was a single-center, prospective cohort study that included all patients >18yo who were intubated and mechanically ventilated in a large volume (90k yearly visits) academic center in St. Louis. Data from June 2019 through May 2020 were included in the study.
The primary outcome was the incidence of being awake while paralyzed. The Brice Questionnaire, which has been used extensively in the prior anesthesia work in this area, was used to assess consciousness following paralysis. Three reviewers independently reviewed the questionnaires to determine yes/possible/no to whether the patient was awake while paralyzed.
Those who died, had severe neurologic injury, were lost to attrition, or transferred were excluded.
But wait, “Awake and Paralyzed” is subjective; how do you “measure” it?
The Brice Questionnaire has been validated extensively in the anesthesia literature. Specifically, question #3 is critical. “Can you remember anything between LOC and waking?” The patients had to report a sensation of wakeful paralysis AND have had administration of neuromuscular blockade to qualify. The questioning occurred after extubation and before hospital discharge. After reviewing the patient’s answers, the independent investigators graded the possibility of awake paralysis as “No, Possible, or Definite.” Complete patient survey answers were included in the manuscript, and the authors were cautious to handle the results as conservatively and transparently as possible. There was ultimately good agreement between the three investigators as the intraclass correlation coefficient was 0.72.
What Else Do We Know About being awake while sedated?
As mentioned earlier, the majority of the literature in the area comes from the OR setting. Does it even matter if someone experiences this? That is a dumb question, but yes, up to 70% of cases develop long-term severe psychiatric problems (PTSD). Remember these numbers for later – 0.1-0.2% incidence of being awake and paralyzed occurs in the OR setting. What increases the risk in the OR? IV anesthesia, underdosing sedatives, long-acting neuromuscular agents (rocuronium) all increase the risk of awake paralysis. SOUND FAMILIAR?? THESE ARE ED/EMS INTUBATING CONDITIONS.
Has anybody looked at this in the ED? There are four studies with a combined n=123 using non-validated and non-standardized questions, emphasizing the need for additional work.
The Results
There were 833 patients intubated in the ED during the study period. Four hundred fifty were excluded, leaving 383 for final analysis. 10/383 (2.6%) of study patients were determined to be possibly or likely awake while sedated. 70% of the ten awake paralyzed patients got rocuronium vs. only 31% of the other 373 patients in the study. This yields an odds ratio of 5.1 (95% CI 1.3 – 20) for rocuronium exposure.
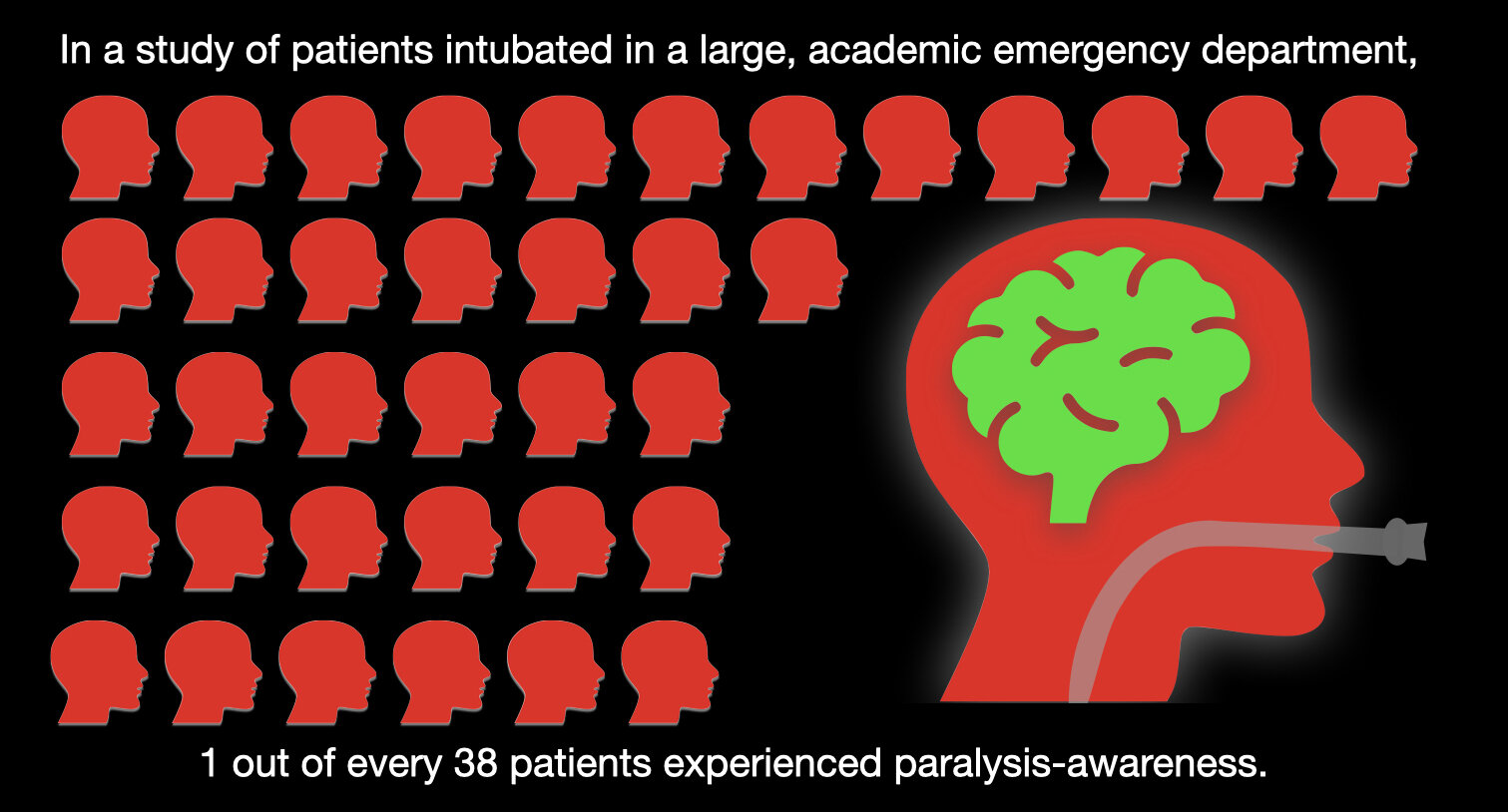
To summarize, the investigators found 3x the rate of awake paralysis in the ED following intubation as compared to the highest risk OR patients (the actual value may be higher than 2.6%, as they handed their data as conservatively as possible).
Let’s put the “data” aside and talk about some of the patient stories…
• “I remember the breathing tube going in.”
• “I remember them putting the breathing tube down, but I could not move.”
• “It was terrible and traumatic – I was panicking inside.”
• “I remember waking up with someone pulling my injured leg, I tried to move, but I could not” – ED records noted a “spike in BP.”
• “For a minute, the patient experienced paralysis in which she couldn’t move anything, including her eyes.”
• “When I woke up, I could not move but could hear people talking about putting a camera down to look in my lungs.”
• “I had a breathing tube in my throat and tried to move and talk but could not.”
What Should We Do Now?
We teach post-intubation sedation in the EMS world, and most services do an excellent job. EMS paralysis and sedation occur entirely via the IV/IM route. The continued trend from succinylcholine to rocuronium use is likely not slowing for other exceedingly valid reasons. So, prehospital intubations, just like those in the ED, are awake paralysis risk factors from the start. That said, a second post-intubation dose of sedative MUST be protocolized when using paralytic medication in both the field and the ED.
The Bottom Line …
The rate of being awake and paralyzed in the emergency department following intubation is likely 3x that which occurs in the operating room setting. Patients who experience this have substantially increased risks of subsequent mental health problems like PTSD. This study is a vital reminder of why adequate sedation is essential and why thorough and continuous QI/QA of EMS paralyzed patients is imperative. Let’s not get lax; one awake patient following paralysis and intubation is too many.
EMS MEd Editor & Image Credit: Maia Dorsett, MD PhD FAEMS, @maiadorsett



