Article Summary by Michael DeFilippo, DO
Background:
Ventricular fibrillation (VF) remains a dire situation in cardiac arrest, especially when refractory to conventional treatment modalities such as CPR and standard defibrillation (anterior-posterior, or anterior-lateral). Refractory VF is defined as an initial presenting rhythm of VF or pulseless ventricular tachycardia that remains present after three consecutive rhythm analyses and standard defibrillations separated by 2-minute intervals of CPR. A pivotal study on managing refractory VF, “Defibrillation strategies for refractory ventricular fibrillation” was published in the New England Journal of Medicine in 2022, and introduced groundbreaking, evidence-based approaches that surpass the constraints of traditional defibrillation methods, presenting new possibilities for treatment in this subset of cardiac arrest patients.
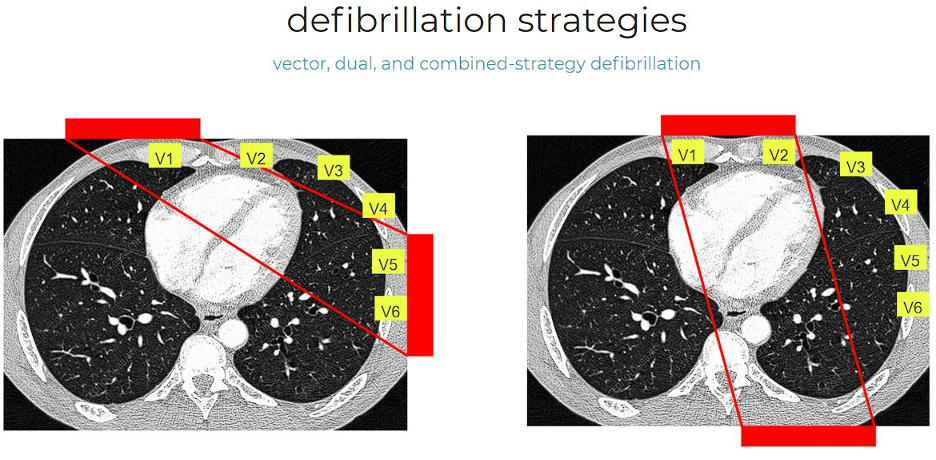
Vector change (VC) defibrillation involves altering the placement of defibrillation pads from the standard anterior-lateral position to an anterior-posterior configuration, potentially targeting different myocardial areas and enhancing the effectiveness of the shock. Dual sequential defibrillation (DSED) entails the delivery of two near-simultaneous defibrillation shocks from two separate defibrillators (one placed anterior-lateral and one placed anterior-posterior), aiming to increase the energy and area covered by the shock, thereby improving the chances of terminating refractory ventricular fibrillation.
Patient Selection
The study included 405 patients experiencing refractory VF during out-of-hospital cardiac arrests, conducted across six Canadian paramedic services. Selection criteria identified patients who still exhibited refractory VF after three consecutive standard defibrillation attempts, intentionally excluding those with cardiac arrests of traumatic origin or who had advance directives against aggressive resuscitation. This approach allowed for a detailed investigation into refractory VF, examining the effectiveness of defibrillation methods across varied patient demographics. Within this cohort, 136 patients were assigned to standard defibrillation, 144 to VC defibrillation, and 125 to DSED, facilitating a comparative analysis of the outcomes associated with each method.
Pertinent Findings
Statistically significant findings from the study indicated a notable improvement in both neurologically intact survival and overall survival for patients treated with DSED and VC defibrillation techniques compared to standard methods. Specifically, survival to hospital discharge was significantly higher in the DSED group at 30.4%, compared to 13.3% in the standard defibrillation group. The VC defibrillation group also showed improved survival rates to hospital discharge at 21.7% versus 13.3% in the standard group. Importantly, DSED was associated with a higher incidence of favorable neurological outcomes, indicating an enhanced quality of survival for these patients. These findings underscore the potential of DSED and VC defibrillation to significantly impact patient outcomes positively, in particular with neurologically intact survival.
Takeaways
The study underscores a pivotal advancement in treating refractory VF, evidencing that both DSED and VC defibrillation outperform standard methods in improving survival and neurological outcomes. These results advocate for EMS protocols to be revised and broadened to encompass DSED and VC defibrillation, potentially enhancing the effectiveness of on-scene management and increasing survival and recovery rates in high-risk patient groups. However, as the Sasson and Haukoos editorial articulates, this enthusiasm must be tempered with prudence. The study’s premature conclusion due to COVID-19 challenges, coupled with a resultant smaller participant pool, signals the need for additional research to validate these findings across more diverse populations. Furthermore, the lack of comprehensive data on post-resuscitation care introduces uncertainty about the standalone impact of these innovative defibrillation techniques. This highlights the critical need for integrating these strategies within a holistic post-resuscitation care framework to accurately gauge their effectiveness. EMS systems, while contemplating the inclusion of DSED and VC defibrillation into their protocols, must also acknowledge the ongoing requirement for rigorous investigation. EMS systems are encouraged to consider these evidence-based findings in their ongoing efforts to optimize emergency cardiac care and improve patient outcomes with the understanding that further research is still needed in this emerging area of resuscitation research.
Editing by James Li, MD NAEMSP Blog Editor



