by Al Lulla, MD (@al_lulla) and Bridgette Svancarek, MD
Expert/Peer Reviewed by J. Brent Myers, MD, MPH (@bmyersmd)

You arrive on scene to a cardiac arrest. Your patient is a 64 yo male found pulseless by his wife when she returned from walking the family dog. The patient’s initial rhythm was a narrow complex PEA. Twenty-five minutes and 12 cycles of CPR later the rhythm remains unchanged. The man’s wife is distraught and tearful. Your clinical experience tells you that the likelihood of a good outcome is poor.
Termination of resuscitation (TOR) is commonplace in the ED and ICU setting, but there is a role for TOR in the pre-hospital setting as well. When is it appropriate to do so? What are the risks and benefits of such this decision?
Literature Review
Nontraumatic out of hospital cardiopulmonary arrest (OHCA) is considered to be a catastrophic event that is associated with a poor prognosis. According to a report published by the American Heart Association, it is estimated that there is an annual incidence of 326,000 OHCAs occurring in the United States [1]. Several studies have reported that for the majority of patients, only those who regain pulses in the field may end up surviving to hospital discharge. For patients who do not regain pulses, outcomes are generally poor. Bonnin, et al. reported a 0.6% survival rate in patients who did not achieve return of spontaneous circulation (ROSC) within 25 minutes of paramedic arrival [2]. Another study performed in Japan demonstrated that death was 25.8 times more likely in patients without prehospital ROSC [3]. Despite these dismal statistics, in attempt to maximize chance for survival, patients who have suffered an OHCA are often continuously resuscitated by EMS and transported to the ED.
In 2011, the National Association of EMS Physicians (NAEMSP) released a position statement regarding termination of resuscitation in patients with non-traumatic cardiopulmonary arrest. In the statement, the NAEMSP affirmed the following:
… As there are patients who will not be successfully resuscitated, an evidence-based methodology to determine those patients with out-of-hospital non traumatic cardiopulmonary arrest that will not result in a favorable outcome would contribute to the public health by conserving valuable health care resources and decreasing the number of emergency vehicles in transit with warning lights and sirens.
In addition to the poor outcomes associated with OHCA, the NAEMSP position statement touches upon several points that favor TOR versus transporting patients [4]:
· Lights and sirens can be dangerous: According to the National Highway Traffic Safety Administration (NHTSA) Fatality Analysis System, approximately 59.6% of ambulance crashes occur during emergency use. Another study identified 45.9 ambulance crashes per 100,000 patients with lights and sirens versus 27.0 ambulance crashes per 100,000 patients without lights and sirens [5].
· High quality CPR: Guidelines put forth by the American Heart Association highlight the importance of high quality CPR. There is some evidence to suggest that on scene chest compressions are higher quality in comparison to compressions done en route. Russi, et al. evaluated quality of chest compressions on scene vs transport in 140 patients. The study reported significantly lower quality compressions (i.e. decreased depth) during transport versus on scene. [6]
· Financial cost and resource depletion: The cost of an unsuccessful resuscitation is significant, especially given scarce EMS resources. In addition, there is a cost to the general public when an EMS crew is out of service transporting a patient. For EMS physicians and providers in the field, it’s important to ask: is continuing resuscitation in the best interest of the patient?
The points highlighted by the NAEMSP position paper as well as pre-hospital research which confirms poor outcomes for OHCA have served as an impetus for the implementation of TOR criteria in EMS systems. While multiple different sets of criteria have been studied and subsequently validated, by far the most widely accepted and researched were the criteria put forth by the Ontario Prehospital Advanced Life Support (OPALS) group.

From their registry of cardiac arrest patients, the OPALS investigators derived two sets of TOR rules, one for basic life support (BLS) providers and one for advanced life support (ALS) providers. These rules were retrospectively developed based on the goal of identifying all non-survivors. The BLS rule included three criteria of which all need to be fulfilled in order to terminate the resuscitation: unwitnessed by EMS, no AED or shock delivered, and no ROSC. The ALS criteria included the BLS rules and two additional criteria: the arrest had to be unwitnessed by a bystander, and no bystander CPR was performed.
The data from the OPALS cardiac arrest registry showed that patients who fulfill all of the TOR criteria do not have good outcomes. For the BLS TOR protocol, Verbeek et al reported the rule to be 100% sensitive in identifying survivors and had a negative predictive value of 100% in identifying non-survivors in patients with OHCA [7]. These findings were validated in subsequent studies. Sasson, et al. demonstrated in a retrospective cohort study that in 2592 patients who suffered from OHCA and met BLS TOR criteria, only 0.2% survived to hospital discharge (98.7% specificity, CI 97.0-99.6). In the 1192 patients who met ALS TOR criteria, 0 survived to hospital discharge (100% specificity, CI 99.1-100). In essence both rules have close to 100% positive predictive value for predicting death in patients with OHCA [8].
Morrison, et al. had similar findings in their study, which just looked at BLS termination criteria regardless if there were BLS or ALS providers on scene. They found that in 776 patients who fulfilled BLS TOR criteria, only 4 patients (0.5%) survived, with a positive predictive value of 99.5% for predicting death. Of the 4 survivors, 3 were characterized as having good cerebral performance, with 1 patient having severe neurological disability. The study showed that implementation of the BLS TOR criteria would theoretically reduce rate of transport by 62.6%! How to reconcile this benefit with three neurologically-intact survivors who met BLS TOR criteria was not explicitly addressed. [9]
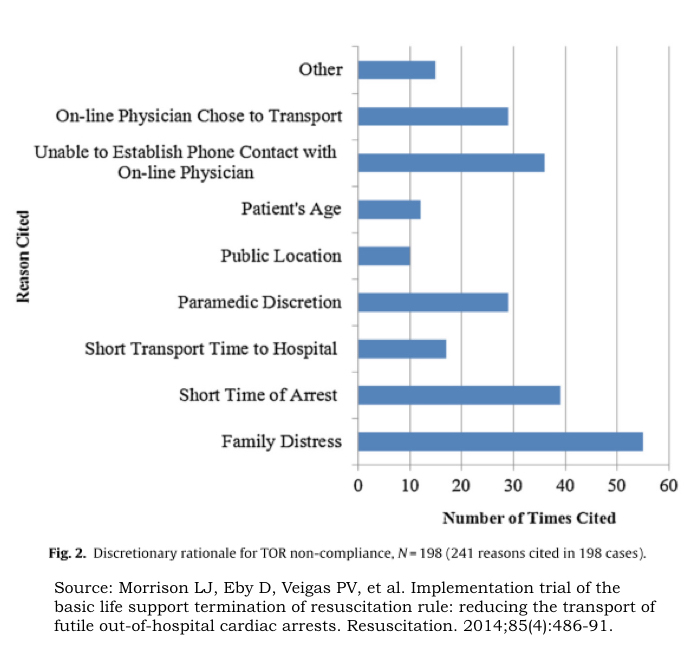
No matter which way you look at it, the research on pre-hospital TOR is clear: OHCA patients who fulfill BLS or ALS TOR criteria most often do not survive to hospital discharge. Studies consistently show a survival of less than 0.5% if BLS TOR criteria are followed and 0% if ALS criteria are followed. Studies also show transportation rates of 40-60% if BLS criteria are followed and around 80% if ALS criteria are followed. In spite of this, research suggests that there are barriers to the implementation of TOR criteria by EMS providers. The Termination of Resuscitation Implementation Trial (TORIT) was a multi-center prospective trial that evaluated the implementation of TOR rules in patients with OHCA. The investigators showed that in 953 patients who were BLS TOR eligible, EMS providers correctly applied the rule in 755 patients (79%) and did not apply the rule in 198 patients (21%). All of the 198 patients in whom the rule was not applied (i.e. they were transported to the hospital despite meeting BLS TOR criteria) did not survive. For these patients, providers were surveyed regarding their decision to transport. Family distress was the most commonly cited reason for continuing resuscitation and transporting patients [10].
Is there a magic number?
Studies have shown that pre-hospital ROSC is the most important predictor of survival for patients with OHCA. An important question often arises: how long should EMS providers work these patients in the field? The prospective 1993 study by Bonnin, et al. showed that in 1471 patients with OHCA, only 370 patients achieved ROSC on scene. Of these 370 patients, all patients achieved ROSC within 25 minutes of paramedic arrival. Newer research coming out of Wake County EMS has shown that working patients longer may be of benefit. In 2905 adult OHCA patients that were examined retrospectively, 363 survived (12.5%). Of the survivors, 300 patients (83%) were neurologically intact. The investigators found that duration of prehospital resuscitation was less than 40 minutes in 90% of neurologically intact survivors [11]. Other studies have shown neurologically intact survival with duration of resuscitation times ranging between 35 to 60 minutes. This broad range may likely be attributed to variation in EMS practice and available resources (i.e. therapeutic hypothermia) as it pertains to agency specific protocols for OHCA.
And what about traumatic cardiopulmonary arrest?
Prehospital TOR may also play a significant role in patients suffering from traumatic arrest as well. While there are sets of robust decision rules validated for TOR and nontraumatic cardiopulmonary arrest, the research on TOR in traumatic arrest patients is scarce.
In 2012, the NAEMSP in conjunction with the American College of Surgeons Committee on Trauma (ACSCOT) released a joint position statement addressing this issue. Based on a review of the literature, the NAEMSP-ACSCOT paper estimated that survival rates for traumatic cardiopulmonary arrest is approximately 2%. This position paper differentiates between withholding resuscitation in cardiopulmonary arrest and TOR.
The guidelines recommend withholding resuscitation in the following patients with traumatic arrest [12]:
· Whom death is the predictable outcome
· Injuries incompatible with life (i.e. decapitation, hemicorporectomy)
· Blunt or penetrating trauma with evidence of prolonged cardiac arrest (i.e. rigor mortis)
· Blunt trauma patients who are apneic, pulseless, without organized EKG activity
· Penetrating trauma patients who are apneic without signs of life (i.e. no spontaneous movement, EKG activity, pupillary response)
The paper makes the following comments regarding TOR in traumatic arrest:
· The primary focus should be evacuation to an appropriate facility for definitive care
· EMS systems should implement protocols that allow for TOR in cases of traumatic arrest
· TOR should be considered in patients without signs of life or without ROSC
· Protocols should be in place that require for a specific interval of CPR (for example, up to 15 minutes prior to termination)
· TOR protocols should be accompanied by procedures to ensure appropriate management of the deceased patient and support services for family members
· Physician oversight is a mandatory component of TOR protocols
· TOR protocols should include locally specific clinical, environmental or population based situations for which the protocol may not be applicable
· Further research is required to determine optimal duration of CPR before TOR
A criticism of the NAEMSP-ACSCOT guidelines is their degree of detail and likely inability to be implemented in the field. A recent paper published in 2016 from Taiwan looked at a simplified decision rule for TOR in patients with traumatic cardiopulmonary arrest modified from the NAEMSP-ACSCOT guidelines. The simplified decision rule included two criteria: 1) blunt trauma injury AND 2) presence of asystole. The study found that this TOR rule could accurately predict 100% of non-survivors and had the potential to decrease ambulance transports for traumatic cardiopulmonary arrest between 16.4-29.0% [13].
Take home points
· The majority of patients with nontraumatic OHCA who do not achieve ROSC in the field have a very poor prognosis
· Identifying patients with OHCA who will most likely have an unfavorable outcome and not benefit from transport with lights and sirens is important with regards to EMS safety and utilization.
· The BLS and ALS TOR criteria derived from the OPALS cardiac arrest registry have been validated and are good predictors for which patients can be pronounced dead in the field
· TOR may have an important role in patients suffering from traumatic arrest, however further research is still needed
· There is still no widely accepted guidelines in terms of duration of prehospital resuscitation for OHCA, however several studies have shown successful outcomes ranging from 25 to 60 minutes
· There are still barriers to implementation of TOR criteria which may explain underutilization by EMS agencies. As family distress is the most commonly cited region for falling out of protocol, additional training of EMS personnel in communication skills, as well as public education will be important to successful implementation.

EMS MEd Editors: Maia Dorsett (@maiadorsett) & Hawnwan P. Moy (@PECpodcast)
References:
1. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29-322.
2. Bonnin MJ, Pepe PE, Kimball KT, Clark PS. Distinct criteria for termination of resuscitation in the out-of-hospital setting. JAMA. 1993;270(12):1457-62.
3. Goto Y, Maeda T, Goto YN. Termination-of-resuscitation rule for emergency department physicians treating out-of-hospital cardiac arrest patients: an observational cohort study. Crit Care. 2013;17(5):R235.
4. Millin MG, Khandker SR, Malki A. Termination of resuscitation of nontraumatic cardiopulmonary arrest: resource document for the National Association of EMS Physicians position statement. Prehosp Emerg Care. 2011;15(4):547-54.
5. Saunders CE, Heye CJ. Ambulance collisions in an urban environment. Prehosp Disaster Med. 1994;9(2):118-24.
6. Russi CS, Myers LA, Kolb LJ, Lohse CM, Hess EP, White RD. A Comparison of Chest Compression Quality Delivered During On-Scene and Ground Transport Cardiopulmonary Resuscitation. West J Emerg Med. 2016;17(5):634-9.
7. Verbeek PR, Vermeulen MJ, Ali FH, Messenger DW, Summers J, Morrison LJ. Derivation of a termination-of-resuscitation guideline for emergency medical technicians using automated external defibrillators. Acad Emerg Med. 2002;9(7):671-8.
8. Sasson C, Hegg AJ, Macy M, et al. Prehospital termination of resuscitation in cases of refractory out-of-hospital cardiac arrest. JAMA. 2008;300(12):1432-8.
9. Morrison LJ, Visentin LM, Kiss A, et al. Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2006;355(5):478-87.
10. Morrison LJ, Eby D, Veigas PV, et al. Implementation trial of the basic life support termination of resuscitation rule: reducing the transport of futile out-of-hospital cardiac arrests. Resuscitation. 2014;85(4):486-91.
11. Bachman MW, Williams JG, Myers JB, et al. Duration of prehospital resuscitation for adult out-of-hospital cardiac arrest: Neurologically intact survival approaches overall survival despite extended efforts. Prehosp Emerg Care. 2014;18(1):134–135.
12. Hopson LR, Hirsh E, Delgado J, et al. Guidelines for withholding or termination of resuscitation in prehospital traumatic cardiopulmonary arrest: a joint position paper from the National Association of EMS Physicians Standards and Clinical Practice Committee and the American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2003;7(1):141-6.
13. Chiang WC, Huang YS, Hsu SH, et al. Performance of a simplified termination of resuscitation rule for adult traumatic cardiopulmonary arrest in the prehospital setting. Emerg Med J. 2016;



