by Brandon Bleess, MD
EMS MEd Editor: Maia Dorsett, MD PhD (@maiadorsett)
Case Scenario #1

EMS is dispatched to scene of a witnessed cardiac arrest. A 54 yo male was at a family gathering when he suddenly clutched his chest prior to collapsing and becoming unresponsive. First responders arrived within 4 minutes of initial call to find a bystander attempting CPR. On ALS arrival, first responders are performing compressions, have applied a monitor and shocked once for ventricular fibrillation. Cardio Cerebral Resuscitation (CCR) is continued as patient deteriorates into asystole. He has continuous CPR performed with a supraglottic airway placed as well as epinephrine given every 3-5 minutes and resuscitation is continued for 20 minutes. The paramedic performs a cardiac Point of Care Ultrasound (POCUS) and finds the following:
Cardiac Standstill on Point-of-Care Cardiac Ultrasound
Case Scenario #2
EMS is dispatched to a vehicle motor vehicle collision (MVC). Upon arrival EMS finds significant intrusion into the driver’s side of a vehicle that has been T-Boned by another vehicle. The fire department is finishing extrication of the patient. He is responsive to verbal stimuli and follows commands. He has a heart rate of 122 and blood pressure of 120/56. Given the noise level on scene, the paramedic is unable to auscultate lung sounds in any fields. The patient complains of abdominal pain and a seat belt sign is noted. Local protocols state to transport to the closest facility, however the astute paramedic knows that the patient could be better served at a trauma center if surgery is needed. Noting his vital signs and exam, he knows that intraperitoneal hemorrhage, tension pneumothorax, or pericardial effusion could be the cause of his presentation. The paramedic performs a eFAST exam and finds the following:
Free Fluid in the Right Upper Quadrant on FAST exam
Normal Lung Slide
POCUS has improved the clinical practice of emergency medicine, begging the question of whether it should be incorporated into prehospital care. Is POCUS practical for prehospital use? How may it be used for triage and/or clinical management in the prehospital setting?
Literature Review:
The use of ultrasound to improve clinical decision-making and management has ventured out of hospitals and into the prehospital realm. In some clinical scenarios, including cardiac arrest and trauma triage, decreasing “time to ultrasound” may accelerate clinical decisions or lead to more appropriate utilization of healthcare resources.
POCUS in Prehospital Management of Cardiac Arrest
Recent changes in management of Out-of-Hospital Cardiac Arrest (OHCA) from “load and go” to the “stay and play” method of cardiocerebral resuscitation (CCR) have shifted the burden of termination of resuscitation onto prehospital providers. Multiple studies have addressed whether Point-of-Care Cardiac ultrasound would be useful in prehospital management of OHCA [1].
For example, a prospective study of 88 patients in cardiac arrest (PEA or asystole) conducted in Germany published in 2010 evaluated the prognostic value of cardiac ultrasound in OHCA. Among patients with cardiac activity, 34% of patients survived to hospital admission compared to only 6% of those without cardiac activity on initial ultrasound [2]. They did not report survival to hospital discharge or neurologically-intact survival.
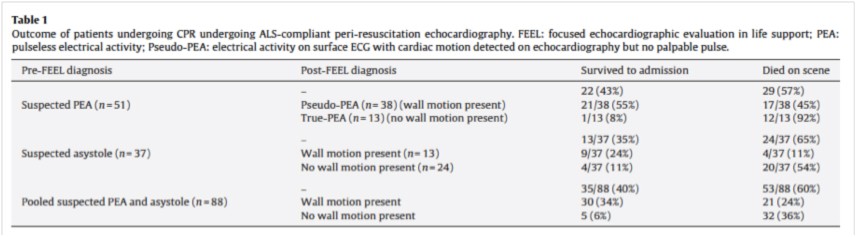
Another small prehospital study published in 2012 enrolled 42 patients in cardiac arrest with any rhythm [3]. Among 32 patients with no cardiac activity on initial field echocardiogram, only one survived to hospital admission. In contrast, 4 of the 10 patients with cardiac activity survived to hospital admission. Only one of forty-two patients survived to hospital discharge (and did so with full neurology recovery). He had cardiac activity on his prehospital ultrasound.
While these results were interesting, both studies were underpowered to detect the key outcome of neurologically-intact survival without cardiac activity on ultrasound due to the overall low incidence of survival from OHCA.
However, an adequately-powered multi-center Emergency Department study of 993 pre-hospital and ED patients with cardiac arrest in PEA or asystole was recently published [4]. Lack of cardiac activity portended an extremely poor likelihood of survival to hospital discharge (0.6%, neurologic status not reported). In addition, POCUS was able to identify causes (Pulmonary embolism, cardiac tamponade) of cardiac arrest not amenable to traditional ACLS interventions.
Given high utilization of resources with prolonged resuscitation and the potential to identify reversible causes of cardiac arrest, these results suggest that cardiac ultrasound may be beneficial in prehospital management of OHCA.
The FAST Exam and Trauma Triage
In emergency department patients with torso trauma, performing a FAST exam decreases time to operative care and the number of CT examinations of the torso [5]. FAST and eFAST (FAST + lung ultrasound) have since become key clinical decision making tools in the triage and management of trauma patients in the ED. Extrapolating this to the field, could early identification of free fluid on abdominal exam better delineate which patients require one trauma center versus another? Could lung ultrasound be used to help identify who needs needle decompression versus who does not, thus avoiding unnecessary intervention?
The prehospital FAST exam may allow for more appropriate transport destination decisions by providing valuable information to be obtained[6,7,8]. One prospective, multicenter study carried out in Germany study sought to compare the accuracy of physical exam and prehospital FAST exam to detect hemoperitoneum and to determine whether it changed clinical management [9]. They enrolled 230 patients with blunt trauma. Among 202 patients who were fully scanned and were not lost to follow-up, 28 patients were found to have hemoperitoneum by ED ultrasound or CT imaging. 26 of these were identified prehospital, leading the authors to conclude that prehospital FAST has a sensitivity of 93 % (95 % CI 76 – 99 %) and specificity of 99 % (95% CI 97 -100 %). However, as the study excluded patients lost to follow-up or in whom ultrasound was too technically difficult, the sensitivity of prehospital FAST for accurate detection of hemoperitoneum could be falsely inflated. The study was interesting in that the there were several examples where prehospital detection of abdominal free fluid changed patient management, including minimizing prehospital interventions and alerting the receiving hospital to reduce time to surgical intervention. As this was not a randomized trial, it was unclear whether this actually changed to the time to surgical intervention, but based on results of ED-based studies it is likely to have done so.
Several systematic reviews have examined the current evidence regarding the potential usefulness of prehospital ultrasound to change diagnosis or treatment of trauma patients [10,11]. Their overwhelming conclusion? The evidence is promising, although the quality of evidence very low and more studies are needed.
Practical for prehospital use?
Development of handheld, battery-powered, low-weight US machines has created the possibility of bringing US to the prehospital setting. In addition, field ultrasound images can be transmitted en route to the emergency department (ED) similar to 12 lead EKGs [12,13,14].
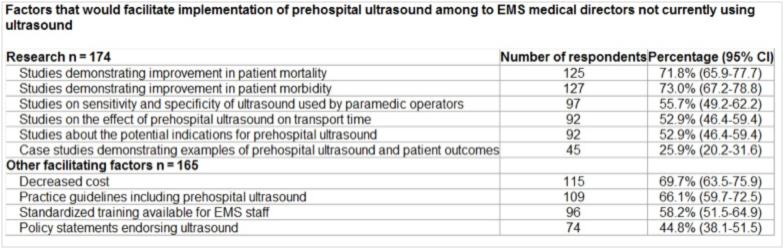
A 2014 survey of medical directors using the NAEMSP mailing list demonstrated that 4.1% of EMS systems were already using ultrasound and that an additional 21.7% of systems were considering the implementation of pre-hospital ultrasound [15]. The vast majority cited equipment costs (89.4%), as well as training costs (73.7%), and challenges related to the training process (53.5%) as the major points of concern of why they the medical directors thought that it could not be implemented in their system.

As a corollary to this, it is not surprising to see that medical directors would be willing to implement ultrasound into their system if there was decreased cost (69.7%), practice guidelines that included prehospital ultrasound (66.1%), a
nd studies demonstrating improvement in patient morbidity (73%) and mortality (71.8%).
Prehospital POCUS use has been more thoroughly investigated in Europe than in the United States [16,17]. This is somewhat of a confounding issue given that many EMS services and Europe use physicians in the field compared to the paramedic model in the United States. So, is training paramedics to accurately perform prehospital POCUS feasible? The current evidence suggests that it is.
Ultrasound education centers on two related but distinct skills: Image acquisition and Image Interpretation.
A 2015 study examined the ability of US EMS Providers’ (EMT, Paramedics, and Students) to interpret ultrasound images and identify pericardial effusion, pneumothorax, and cardiac standstill [18]. They were given a pre-test followed by an hour didactic session covering scanning techniques, normal anatomy, and image interpretation of both normal and pathologic videos. After the didactic they were given an immediate post-test as well as a post-test one week later.
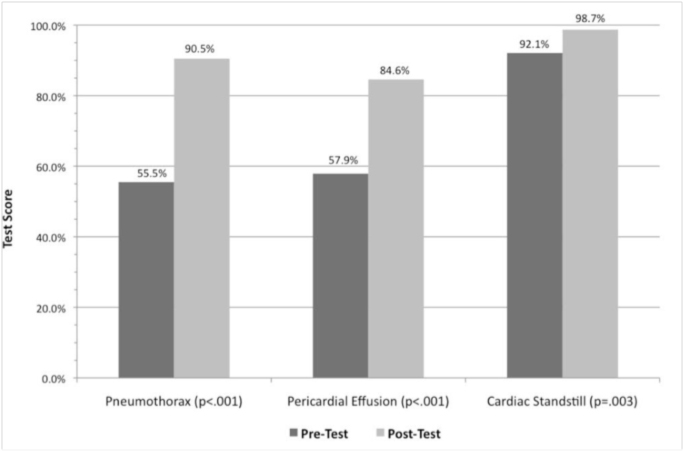

The study found that following a short educational intervention, paramedics could more accurately and confidently identify key ultrasound findings that would affect clinical management. While this study only looked at image recognition and not image acquisition, it showed that the US EMS providers are able to identify pathologic conditions on ultrasound.
Several studies have examined educational programs to train paramedics to both acquire and interpret prehospital ultrasound images.
A 2010 study looked at US paramedics and their ability to perform and interpret FAST exams and abdominal aortic (AA) exams [19]. Paramedics from two EMS agencies received a 6 hour training program with ongoing refresher education. All ultrasound exams were then reviewed by a blinded physician overreader (PO). A total of 104 patients were evaluated (84 FAST and 20 AA) using ultrasound, of which 76 FAST exams were adequate for evaluation and all 20 AA exams were adequate. Of that, 6 FAST exams were deemed positive by the paramedics and the PO. All 20 of the AA exams were deemed negative by the paramedics and the PO. With these, there was a 100% proportion of agreement between the paramedics and the PO. The study also looked at the amount of time that it would take paramedics to perform the exams as this could be a possible downside prior to transport. The mean time for image acquisition for the FAST exam was 156 seconds (2.6 minutes) with the median being 138 seconds (range of 76-357 seconds).
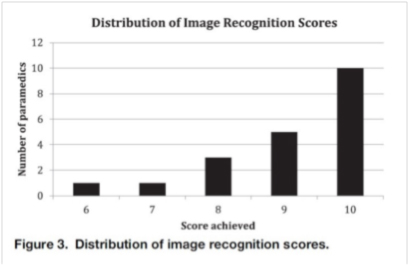
Figure 3, PAUSE study (Ref 20)
A 2013 study looking at the viability of a Prehospital Assessment with Ultrasound for Emergencies (PAUSE) Protocol enrolled 20 firefighter/paramedics that did not have prior ultrasound training. They underwent a 2 hour didactic session on the use of ultrasound on the lungs and heart to look for pneumothorax, pericardial effusion, and cardiac activity [20].
As noted in Figure 3 from the PAUSE study, 18 of the 20 subjects scored an 80% or higher and the mean score was 9.1 overall.
There was one image of cardiac standstill that 6 of the 20 paramedics answered incorrectly. The authors note that the believed this to be due to the perceived cardiac movements as a result of the ultrasound probe being moved across the patient’s chest.

When evaluating image acquisition, 100% of the images for the evaluation of pneumothorax were noted to be satisfactory. The Cardiac Ultrasound Structural Assessment Scale (CUSAS) was used to assess for adequate cardiac views for diagnosis [21]. The authors noted that for the purposes of determining cardiac standstill, being able to visualize any myocardium (CUSAS Score 3) should be adequate. If this is true, there is a 100% success rate in the study. They also believed that a significant pericardial effusion causing tamponade would likely be seen with CUSAS score of ≥4, as these images offer at least a partial view of the pericardium. Given these assumptions, in this study, 95% of the participants (19/20) were able to quickly acquire images that would likely be useful in assessing for both cardiac activity and a pericardial effusion. In terms of time, views of the lung were acquired in less than 5 seconds. The views of the heart were acquired in less than 10 seconds for 16 paramedics. One paramedic took approximately 90 seconds, and the other three ranged between 10 and 25 seconds.
Take Home
In the hands of physicians and paramedics, POCUS is a promising technology to direct clinical care and utilization of prehospital resources. However, the use of prehospital ultrasound must improve patient outcomes for it to become a reality and the standard of care.
Credits
Videos courtesy of Washington University in St. Louis Division of Emergency Medicine, Section of Emergency Ultrasound.
References
1. Kellum MJ, Kennedy KW, Barney R, et al. (2008) Cardiocerebral resuscitation improves neurologically intact survival of patients with out-of-hospital cardiac arrest. Ann Emerg Med;52:244–52.
2. Breitkreutz, R., Price, S., Steiger, H. V., Seeger, F. H., Ilper, H., Ackermann, H., Walcher, F. (2010). Focused echocardiographic evaluation in life support and peri-resuscitation of emergency patients: A prospective trial. Resuscitation, 81(11), 1527-1533.
3. Aichinger, G., Zechner, P. M., Prause, G., Sacherer, F., Wildner, G., Anderson, C. L., Fox, J. C. (2012). Cardiac movement identified on prehospital echocardiography predicts outcome in cardiac arrest patients. Prehospital Emergency Care Prehosp Emerg Care, 16(2), 251-255.
4. Gaspari, R., Weekes, A., Adhikari, S., Noble, V. E., Nomura, J. T., Theodoro, D., … & Caffery, T. (2016). Emergency department point-of-care ultrasound in out-of-hospital and in-ED cardiac arrest. Resuscitation, 109, 33-39.
5. Melniker, L. A., Leibner, E., McKenney, M. G., Lopez, P., Briggs, W. M., & Mancuso, C. A. (2006). Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: the first sonography outcomes assessment program trial. Annals of emergency medicine, 48(3), 227-235.
6. Chaudery, M., Clark, J., Wilson, M. H., Bew, D., Yang, G., & Darzi, A. (2015). Traumatic intra-abdominal hemorrhage control. Journal of Trauma and Acute Care Surgery, 78(1), 153-163.
7. O\’Dochartaigh, D., & Douma, M. (2015). Prehospital ultrasound of the abdomen and thorax changes trauma patient management: A systematic review. Injury, 46(11), 2093-2102.
8. Ruesseler, M., Kirschning, T., Breitkreutz, R., Marzi, I., & Walcher, F. (2009). Prehospital and emergency department ultrasound in blunt abdominal trauma. Eur J Trauma Emerg Surg European Journal of Trauma and Emergency Surgery, 35(4), 341-346.
9. Walcher F, Weinlich M, Conrad G, et al. Prehospital ultrasound imaging improves management of abdominal trauma. Br J Surg. 2006; 93:238–42.
10. Jørgensen, H., Jensen, C. H., & Dirks, J. (2010). Does prehospital ultrasound improve treatment of the trauma patient? A systematic review. European Journal of Emergency Medicine, 17(5), 249-253.
11. O’Dochartaigh, D., & Douma, M. (2015). Prehospital ultrasound of the abdomen and thorax changes trauma patient management: A systematic review. Injury, 46(11), 2093-2102.
12. Sibert, K., Ricci, M. A., Caputo, M., Callas, P. W., Rogers, F. B., Charash, W., . . . Kocmoud, C. (2008). The feasibility of using ultrasound and video laryngoscopy in a mobile telemedicine consult. Telemedicine and E-Health, 14(3), 266-272.
13. Strode, C. A. (2003). Satellite and mobile wireless transmission of focused assessment with sonography in trauma. Academic Emergency Medicine, 10(12), 1411-1414.
14. Takeuchi, R., Harada, H., Masuda, K., Ota, G., Yokoi, M., Teramura, N., & Saito, T. (2008). Field testing of a remote controlled robotic tele-echo system in an ambulance using broadband mobile communication technology. J Med Syst Journal of Medical Systems, 32(3), 235-242.
15. Taylor, J., McLaughlin, K., McRae, A., Lang, E., & Anton, A. (2014). Use of prehospital ultrasound in North America: a survey of emergency medical services medical directors. BMC Emergency Medicine, 14, 6
16. Walcher F, Petrovic T, Heegaard W, et al.(2008) Prehospital ultrasound: perspectives from four countries. In: MAJ, MateerJ, BlaivasM, eds. Emergency Ultrasound. New York, NY: McGraw Hill.
17. Nelson BP, Chason K. Use of ultrasound by emergency medical services: a review(2008). Int J Emerg Med. 1:253–9.
18. Bhat SR, Johnson DA, Pierog JE, Zaia BE, Williams SR, Gharahbaghian L. (2015) Prehospital Evaluation of Effusion, Pneumothorax, and Standstill (PEEPS): Point-of-care Ultrasound in Emergency Medical Services. Western Journal of Emergency Medicine. 16(4):503-509.
19. Heegaard, W., Hildebrandt, D., Spear, D., Chason, K., Nelson, B. and Ho, J. (2010), Prehospital Ultrasound by Paramedics: Results of Field Trial. Academic Emergency Medicine, 17: 624–630.
20. Chin E, Chan C, Mortazavi R. (2013) A pilot study examining the viability of a Prehospital Assessment with UltraSound for Emergencies (PAUSE) protocol. J Emerg.44:142–149.
21. Backlund, B., Bonnett, C., Faragher, J., Haukoos, J., and Kendall, J. (2010) Pilot study to determine the feasibility of training Army National Guard medics to perform focused cardiac ultrasonography. Prehosp Emerg Care. 14: 118–123.
Share:
More Posts
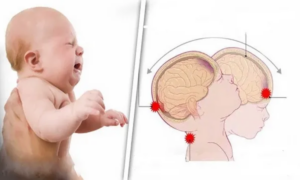
Response to Non-Accidental Trauma and Traumatic Brain Injury in Infants and Young Children
Author: Rachel O’Dell, MD; Washington University Emergency Medicine Residency Editor: Michael DeFilippo, DO As first-responders, EMS personnel are in a unique position to observe and categorize the setting and behaviors of children presenting with possible non-accidental trauma (NAT). However, children, and especially infants, pose a particular difficulty in identifying trauma due to their subtle presentation.

Agitated with a head injury: Will Ketamine make it worse?
Author: Katie Stuart MD; Washington University Emergency Medicine Residency Editors: Sarah Fabiano MD, FACEP, FAAEM & Michael DeFilippo DO You are a second-year emergency medicine resident physician doing a ride along with a helicopter-based EMS (HEMS) agency. You are dispatched to the scene of a golf cart versus tree. The air crew successfully identifies a

The Role of EMS in Palliative Extubation
A review of EMS palliative extubation for patient-centered end of life care
