by Kevin Baumgartner, MD
EMS MEd Editor: Maia Dorsett (@maiadorsett)
Case: EMS is dispatched to the scene of a Motor Vehicle Accident. They arrive to find a 45 year old male who was riding his bicycle when he was hit by a car traveling at approximately 35 mph. Eyewitnesses state that the man was thrown from his bicycle and hit his head on the pavement. On their initial assessment, paramedics find a poorly responsive middle-aged male who will not open eyes spontaneously, makes no verbal response but withdraws to painful stimuli. He has obvious head trauma with a large hematoma and laceration overlying his parietal scalp. The patient has rapid and shallow spontaneous respirations and the paramedics need to decide how to best manage his airway during their twenty minute transport to the local trauma center.
Clinical Question: Do patients with severe traumatic brain injury benefit from prehospital intubation?

Literature Review:
Airway management is a cornerstone of both basic and advanced life support. Paramedics and other EMS providers frequently encounter patients who can no longer protect their own airways (traumatic brain injury, major polytrauma, intoxication and overdose) or who are experiencing impending respiratory failure (exacerbations of congestive heart failure and obstructive lung disease). In-hospital management for these patients typically includes endotracheal intubation (ETI), which provides definitive control of the airway, reduces aspiration risk, and allows for mechanical ventilatory support. Do any of these patients benefit from pre-hospital ETI? Should EMS providers intubate in the field, or should they use airway adjuncts such as bag-valve mask ventilation, supraglottic airway devices, or non-invasive positive pressure ventilation to temporize their patients during rapid transport to the hospital?
As one might expect, the data on this issue are mixed and generally poor in quality. Given the ethical and logistical difficulties involved in designing true randomized controlled trials of field vs. in-hospital ETI, most research has been retrospective and observational. As Pepe and colleagues point out in their 2015 review, patients who are intubated in the field are almost by definition the sickest patients encountered by EMS providers; as such, any naïve univariate analysis will almost certainly find that prehospital ETI is associated with poor outcomes [1].
Pepe and colleagues also note that success of prehospital ETI (and thus overall patient outcomes) is strongly influenced by the type, intensity, and duration of training that is provided for EMS personnel, as well as the structure of the individual EMS service being studied. This intuitive conclusion was reinforced by a 2015 meta-analysis by Bossers and colleagues, which demonstrated that prehospital ETI by EMS providers with “limited proficiency” was associated with increased mortality (OR 2.33, 95% CI 1.61-3.38), while prehospital ETI by EMS providers with “extended proficiency” was not associated with increased mortality [2]. Given the relative rarity of pre-hospital ETI (“critical procedures” including ETI, cardioversion, and defibrillation were performed during only 2.4% of EMS calls in 2011) and the difficulty of allowing a large pool of EMS providers sufficient access to clinical situations requiring ETI, it can be very challenging to allow EMS personnel to acquire the “extended” skills required for routinely successful ETI [1,3].
Pre-hospital ETI has been studied in specific clinical contexts. Severe traumatic brain injury (TBI) frequently robs patients of the ability to protect their own airway from aspiration and oral secretions. Furthermore, every effort must be taken to ensure adequate oxygenation as hypoxia in itself can lead to secondary brain injury and worsen patient outcomes. Unfortunately, the literature is ambivalent on the value of pre-hospital ETI in this population; an abundance of studies suggest that pre-hospital ETI does not improve outcomes, and some suggest that it may actually worsen outcomes. One retrospective cohort study, for example, showed that timing of ETI (pre-hospital vs. in ED) had no effect on mortality in TBI patients [4]. As mentioned above, one large meta-analysis showed no influence of pre-hospital ETI on mortality when ETI was performed by experienced providers [2]. A Californian retrospective case-control study showed that patients with severe TBI managed with pre-hospital ETI had higher mortality and worse admission pO2 than patients who underwent only BLS airway interventions [5]. A cohort-matched retrospective study involving over twenty-seven thousand patients demonstrated that pre-hospital ETI was independently associated with higher in-hospital mortality (OR 1.399, 95% CI 1.205-1.624) [6]. In the OPALS study comparing survival before and after the introduction of Advanced Life support, patients with severe TBI has a lower survival rate during the advanced life-support phase (50.9% vs. 60.0%; P = 0.02) [7]. Indeed, a systematic review of 13 studies on prehospital intubation for TBI published in 2008 found the unadjusted ORs for an effect of pre-hospital intubation on in-hospital mortality varied widely, ranging from 0.17 (95% CI: 0.10–0.31) to 2.43 (95% CI: 1.78–3.33) [8].
While the majority of studies on prehospital intubation for TBI are retrospective or observational, a prospective, randomized control trial of prehospital intubation vs transport and intubation in ED for patients with severe TBI was completed in Australia [9]. The trial included 312 patients with a GCS < 9, evidence of head trauma, age ≥15 years and intact airway reflexes. Patients randomized to undergo prehospital intubation underwent RSI with fentanyl/versed/succinylcholine and subsequent sedation/paralysis with a single dose of pancuronium (0.1 mg/kg), and an intravenous infusion of morphine and midazolam at 5 to 10 mg/h each after confirmation of successful endotracheal tube placement. The primary outcome was neurologic outcome at 6 months post-injury. Using the extended Glasgow Outcome Scale (eGOS) as this measureable outcome, the study found that the median eGOS for patients who underwent prehospital intubation was 5 (moderate disability), while those who underwent hospital intubation had a median eGOS of 3 (severe disability). This difference was not significant (p = 0. 28). There was a significant difference in “good neurologic outcome” (defined as eGOS 5-8) between the two groups (51% prehospital intubation vs. 39% hospital intubation, p = 0.046), but 13 patients were lost to follow-up, the majority of which were in the hospital intubation group. While this study suggests that there may be a benefit of prehospital intubation for patients with severe brain injury, there are important differences between the study and average prehospital practice. First, intubation success rate was 97%. Reports of success rates for prehospital intubation in North America are generally lower, ranging from 83 to 97% [10,11,12]. Second, they had full RSI (sedative and paralytic) as well as post-intubation sedation that would inhibit disadvantageous consequences such as coughing in a severely brain-injured patient.
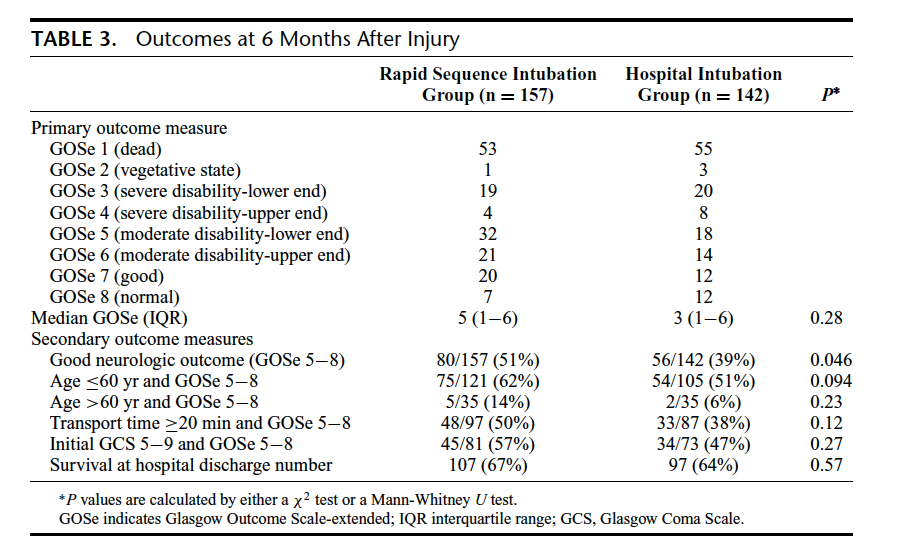
Table 3 from: Bernard, S. A., Nguyen, V., Cameron, P., Masci, K., Fitzgerald, M., Cooper, D. J., … & Patrick, I. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: a randomized controlled trial. Annals of surgery, 2010; 252(6), 959-965

Given the available data, it is reasonable to conclude that pre-hospital ETI in patients with TBI does not improve relevant patient-centered outcomes in most prehospital settings. It is unclear why this is true—possible explanations include delay of transport to definitive care (multiple studies demonstrated increased scene times in patients undergoing ETI), greater willingness on the part of EMS personnel to intubate patients who are overall “sicker,” hypoxia during intubation attempts, hyperventilation leading to decreased cerebral perfusion or simply the high success rate of non-invasive ventilation and oxygenation strategies in this patient population [4,7,13]. At least when it comes to ground transport, where invasive airways are less necessary and overall frequency of intubation as a procedure low, BVM or supraglottic devices may be the preferred method of airway management for patients with severe TBI.
References
1. Pepe et al. Prehospital endotracheal intubation: elemental or detrimental? Crit Care. 2015; 19(1): 121
2. Bossers et al. Experience in Prehospital Endotracheal Intubation Significantly Influences Mortality of Patients with Severe Traumatic Brain Injury: A Systematic Review and Meta-Analysis. PLoS One. 2015; 10(10): e0141034.
3. Carlson et al. Procedures Performed by Emergency Medical Services in the United States. Prehosp Emerg Care. 2016;20(1):15-21.
4. Lansom et al. The Effect of Prehospital Intubation on Treatment Times in Patients With Suspected Traumatic Brain Injury. Air Med J. 2016 Sep-Oct;35(5):295-300
5. Karamanos et al. Is prehospital endotracheal intubation associated with improved outcomes in isolated severe head injury? A matched cohort analysis. Prehosp Disaster Med. 2014 Feb;29(1):32-6
6. Haltmeier et al. Prehospital intubation for isolated severe blunt traumatic brain injury: worse outcomes and higher mortality. Eur J Trauma Emerg Surg. 2016 Aug 27
7.Stiell IG, Nesbitt LP, Pickett W; OPALS Major Trauma Study Group. Impact of advanced life-support on survival and morbidity. CMAJ. 2008;178:1141– 1152.
8. Von Elm, E., Schoettker, P., Henzi, I., Osterwalder, J., & Walder, B. Pre-hospital tracheal intubation in patients with traumatic brain injury: systematic review of current evidence. British journal of anaesthesia, 2009; 103(3), 371-386.
9. Bernard, S. A., Nguyen, V., Cameron, P., Masci, K., Fitzgerald, M., Cooper, D. J., … & Patrick, I. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: a randomized controlled trial. Annals of surgery, 2010; 252(6), 959-965.
10. Bernard S, Smith K, Foster S, Hogan P, Patrick I. The use of rapid sequence intubation by ambulance paramedics for patients with severe head injury. Emerg. Med. 2002; 14: 406–11.
11.Davis DP, Hoyt DB, Ochs M et al. The effect of paramedic rapid sequence intubation on outcome in patients with severe trau- matic brain injury. J. Trauma 2003; 54: 444–53.
12. Wayne MA, Friedland E. Prehospital use of succinylcholine: a 20 year review. Prehosp. Emerg. Care 1999; 3: 107–9.
13.Bernard, S. A. Paramedic intubation of patients with severe head injury: a review of current Australian practice and recommendations for change. Emergency Medicine Australasia, 2006; 18(3), 221-228.