by Adam Rieves, MD (@AdamRieves) and Brandon Bleess, MD (@BBBleess)
EMS MEd Editor: Maia Dorsett (@maiadorsett)
Clinical Scenario: EMS is called to the home of an elderly gentleman with altered mental status. On arrival, they find an elderly male who is muttering to himself. Per his daughter, he has had decreased oral intake and confusion over the last day. His vital signs include a heart rate of 95, blood pressure of 96/40, RR of 32 and an oxygen saturation of 89% on room air. His finger stick blood sugar is 178. The paramedics suspect severe sepsis. Since sepsis is a time-sensitive diagnosis, they wonder whether capnography would be helpful in the care for their patient now and subsequently in the hospital.

Literature Review: The capnograph represents continuous monitoring of the partial pressure of CO2 in a circuit and has four main phases [1]. The first phase (phase 1) represents the end of a breath; this is dead-space ventilation, meaning air that did not participate in gas exchange is cleared from the airways. Phase 2 is a rapid up-tick in the amount of CO2 measured which represents the first gas that is being sampled from the alveoli, i.e. initial exhalation. Phase 3 is known as the “alveolar plateau”. It represents the amount of CO2 in all the alveoli, on average. This plateau should have a slightly positive inclination due to the continuous excretion of CO2 into the alveoli becoming progressively smaller and the late emptying alveoli with a low V/Q ratio containing a relatively higher concentration of CO2. The value displayed on the monitor is equal to the end-tidal CO2 measured at the end of Phase 3. This is when the CO2 concentration reaches a maximum at the end of exhalation and reflects the CO2 concentration of the alveoli emptying last. The last phase (phase 0) of the waveform represents inhalation. Given the change in flow and there is minimal CO2 in the ambient air, the level measured by the detector quickly falls to near zero.
Similar to the role of pulse oximetry in guiding the prehospital provider through both management decisions and differential diagnosis, end-tidal capnography can provide invaluable physiologic information that can be used to enhance prehospital patient care in both intubated and non-intubated patients. .
ETT Placement & Integrity of the Respiratory Circuit
Capnography is the most reliable method to confirm endotracheal tube placement in the pre-hospital setting. In a 2001 study of 345 intubations, capnography had a sensitivity and specificity of 100% for correct placement. It was also found to be better than capnometry (qualitative) given that capnometry had a sensitivity of only 88% in cardiac arrest [3]. This was again demonstrated in a 2005 study of 153 patients intubated in the pre-hospital setting; the incidence of unrecognized esophageal intubations was 0% in patients with continuous EtCO2 monitoring versus 23.3% when continuous EtCO2 monitoring was not used [4].
Beyond initial confirmation of correct placement, capnography provides a continuous assurance of functional tube placement. After initial placement, loss of the waveform can indicate movement of the tube, possible esophageal placement or circuit disconnection. EtCO2 monitoring will also recognize dislodgement or apnea immediately compared to several minutes for the pulse oximeter to recognize desaturation. Given that endotracheal tubes can move upwards of 3 cm with neck extension, patient movement alone can cause tube dislodgement which could go unidentified without continuous EtCO2 monitoring [2]. Therefore, continuous waveform capnography for all patients with an advanced airway can be viewed as standard of care.
Uses in Cardiac Arrest
Because EtCO2 is a surrogate for perfusion, capnography can be used during CPR to monitor the effectiveness of resuscitative efforts. Continuous EtCO2 during resuscitation is associated with an improved rate of ROSC compared to no reported physiologic monitoring [12]. Furthermore, EtCO2>10 mmHg during CPRis associated with improved rates of patient survival to hospital discharge and survival with favorable neurological outcome [12]. A recent meta-analysis of 20 studies determined the average EtCO2 values of patients with ROSC versus those without. This study demonstrated that the mean EtCO2 in participants with ROSC was 25.8 ± 9.8 mmHg versus 13.1 ± 8.2 mmHg in those without ROSC. The mean difference in EtCO2 between those patients who achieved ROSC and those that did not was 12.7 mmHg (95% confidence interval: 10.3-15.1), suggesting that the AHA guidelines of a threshold of 10 to 20 mm Hg during resuscitation may need to be higher [13].
Moreover, EtCO2 is useful in guiding when resuscitative efforts are unlikely to be successful. In 1997 Levine et al. found that in patients with CPR duration > 20 minutes, EtCO2 averaged 4.4 ± 2.9 mmHg (Range 0-10) in non-survivors and 32.8 ± 7.4 mmHg (Range 18-58) in survivors to hospital admission. They also found that a 20-minute EtCO2 value of < 10 mm Hg successfully discriminated between patients who survived to hospital admission and non-survivors. In fact, the sensitivity, specificity, positive predictive value, and negative predictive value were all 100% [8]. This was duplicated in a pre-hospital study by Kolar et al. in 2008 which found thatafter 20 minutes of advanced life support, EtCO2 averaged 6.9 mmHg in patients who did not achieve ROSC and 32.8 mmHg in those who did. A 20-minute EtCO2 value of ≤14.3 mmHg successfully discriminated between ROSC and no ROSC with a sensitivity, specificity, positive predictive value, and negative predictive value of 100% [9]. Reflective of this, the current American Heart Association Guidelines state that, “In intubated patients, failure to achieve an ETCO2 of greater than 10 mm Hg by waveform capnography after 20 minutes of CPR may be considered as one component of a multimodal approach to decide when to end resuscitative efforts but should not be used in isolation.” [10,11]
Metabolic Derangements
DKA
End-tidal capnography has demonstrated great promise for assessment of metabolic derangements. A 2015 research study evaluated end-tidal CO2 as a screening tool for diabetic ketoacidosis (DKA). [14] Among patients presenting to the emergency department with a glucose greater than 550 mg/dL, an EtCO2 ≤ 21 mmHg was 100% specific for DKA. Moreover, an EtCO2 ≥ 35 mmHg allowed DKA to be ruled out with a sensitivity of 100 %. [14] In 2013, Soleimanpour et al. demonstrated that EtCO2 values more than 24.5 mmHg could rule out the DKA diagnosis with a sensitivity and specificity of 90% in patients with a glucose greater than 250 mg/dL [15]. A 2002 study evaluated the usefulness of EtCO2 for identifying acidosis in pediatric patients with hyperglycemia. It demonstrated that EtCO2 is linearly related to HCO3 and is significantly lower in children with DKA. An EtCO2 cut-point of <29 mmHg demonstrated a sensitivity and specificity of 83% and 100% respectively for DKA while an EtCO2 of ≥36 mmHg effectively ruled out DKA. [16]
Severe Sepsis
Severe sepsis and septic shock are time-critical diagnoses. Prehospital activation of a Code Sepsis Alert for patients with severe sepsis has been shown to improve mortality. [17] Severe sepsis is infection with associated end-organ dysfunction – of which one measure of is lactic acidosis due to anaerobic metabolism in the context of poor end-organ perfusion. Several prehospital screens have utilized prehospital lactate, but the lack of availability and prohibitive cost of lactate meters have prevented this from being widely available.
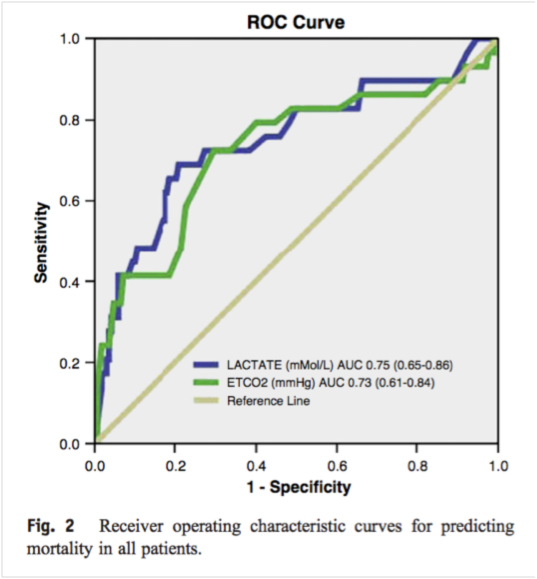
Figures. From Hunter CL, Silvestri S, Dean M, Falk JL, Papa L. End-tidal carbon dioxide is associated with mortality and lactate in patients with suspected sepsis. American Journal of Emergency Medicine. 2013 Jan; 31(1):64-71.
EtCO2 monitoring may serve as a useful surrogate for lactate measurement as it can evaluate for the respiratory compensation in response to the metabolic acidosis. In a 2013 study, Hunter et al. demonstrated that EtCO2 concentration may perform similarly to lactate levels as a predictor for mortality in patients with suspected sepsis [18]. They found an inverse relationship between exhaled EtCO2 levels and serum lactate levels; non-survivors had lower EtCO2 on arrival (26 mmHg) compared to survivors (30 mmHg) [18].
As a follow-up, in 2016 Hunter et al. published a study that evaluated EtCO2 as a component of a prehospital screening tool for sepsis, severe sepsis, or septic shock patients. If the patient met the following criteria: 1. Suspected infection, 2. Two or more of the SIRS criteria (Temperature not between 36°C and 38°C, respiratory rate > 20, heart rate greater than 90) and 3. EtCO2 < 25 mmHg, the ED was notified of a “Sepsis Alert.” This protocol was 90% sensitive, 58% specific and had a negative predictive value of 93% for severe sepsis. Among all prehospital variables, low EtCO2 levels were the strongest predictor of sepsis, severe sepsis, and mortality. There were significant associations between prehospital EtCO2 and serum bicarbonate levels, anion gap, and lactate [19].
MCI Triage
Since the terrorist attacks of September 11, 2001, emergency medical services systems have had continued focus in preparation for a terrorism event causing an MCI. Capnography is a single monitoring modality that can provide assessment of the ABCs in less than 15 seconds. The presence of a normal waveform allows the provider to know that the patient is breathing and the airway is patent. A normal EtCO2 level (35-45 mm Hg) signifies adequate ventilation and perfusion. Furthermore, capnography can allow for rapid assessment of common complications of chemical agents including: apnea, upper airway obstruction, laryngospasm, bronchospasm, and respiratory failure. The absence of the capnogram, in association with the presence or absence of chest wall movement, distinguishes apnea from upper airway obstruction and laryngospasm. Response to airway alignment maneuvers (chin lift, jaw thrust) can further distinguish upper airway obstruction from laryngospasm [6]. Given its usefulness in rapid assessment of the ABCs and ability to identify common complications of chemical terrorism, “EMS systems should consider adding capnography to their triage and patient assessment toolbox and emphasize its use during educational programs and MCI drills.”[7]
Limitations
End-tidal CO2 levels do not necessarily correspond to paCO2 levels obtained on an arterial blood gas. In patients that have abnormal lung function, the gradient will widen depending on the severity of the lung disease. EtCO2 in patients with lung disease, such as an obstructive lung disease, is only useful for trending ventilatory status over time; not as a single number spot check that may or may not correlate with the pCO2 [20,21].
Conclusions
Capnography in EMS has evolved substantially from its origins as a qualitative color change pH indicator to identify successful endotracheal intubation. What once was a tool just for anesthesia in the Operating Room has become a transformative tool in the pre-hospital setting. Uses have evolved to include early recognition of respiratory inadequacy and failure, integrity of the ventilator circuit, identification of a dangerous inhalation and triage, adequacy of resuscitation during cardiac arrest including detection of ROSC, prediction of diabetic ketoacidosis and early identification and treatment sepsis. Given this, capnography has the opportunity to become as indispensable as the cardiac monitor in the pre-hospital management of many conditions.
References
1. Bhavani-Shankar K, Philip JH. Defining segments and phases of a time capnogram. Anesthesia and Analgesia 2000;(4):973-7
2. Kim JT, Kim HJ, Ahn W, et al.. Head rotation, flexion, and extension alter endotracheal tube position in adults and children. Can J Anaesth.2009;56(10):751–756.
3. Grmec S. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Intensive Care Med. 2002;28:701–4.
4. Silvestri S, Ralls GA, Krauss B, et al. The effectiveness of outof-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system. Ann Emerg Med. 2005;45:497–503.
5. Krauss B. Capnography as a rapid assessment and triage tool for chemical terrorism. Pediatr Emerg Care, 2005; 21:493-497.
6. Krauss B. Advances in the Use of Capnography for Nonintubated Patients. Israeli Journal of Emergency Medicine. 2008;8:3–15.
7. Krauss B, Heightman AJ. 15-second triage tool. The use of capnography for the rapid assessment & triage of critically injured patients & victims of chemical terrorism. JEMS. 2006 Jun;31(6):60-2, 64-6, 68.
8. Levine RL, Wayne MA, Miller CC. End-tidal carbon dioxide and outcome of out-of-hospital cardiac arrest. N Engl J Med. 1997 Jul 31;337(5):301-6.
9. Kolar M, Krizmaric M, Klemen P, Grmec S. Partial pressure of end-tidal carbon dioxide successful predicts cardiopulmonary resuscitation in the field: a prospective observational study. Crit Care. 2008;12(5):R115. doi: 10.1186/cc7009. Epub 2008 Sep 11.
10. Hazinski MF, Nolan JP, Aicken R, et al. Part 1: executive summary: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2015;132(16)(suppl 1).
11. Neumar RW, Shuster M, Callaway CW, et al. Part 1: executive summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18)(suppl 2).
12. Sutton RM, French B, Meaney PA, Topjian AA, Parshuram CS, Edelson DP, Schexnayder S, Abella BS, Merchant RM, Bembea M, Berg RA, Nadkarni VM. Physiologic monitoring of CPR quality during adult cardiac arrest: A propensity-matched cohort study. Resuscitation. 2016 Sep;106:76-82. doi: 10.1016/j.resuscitation.2016.06.018. Epub 2016 Jun 24.
13. Hartmann SM, Farris RW, Di Gennaro JL, Roberts JS. Systematic Review and Meta-Analysis of End-Tidal Carbon Dioxide Values Associated With Return of Spontaneous Circulation During Cardiopulmonary Resuscitation. J Intensive Care Med. 2015 Oct;30(7):426-35. doi: 10.1177/0885066614530839. Epub 2014 Apr 22.
14. Bou Chebl R, Madden B, Belsky J, Harmouche E, Yessayan L. Diagnostic value of end tidal capnography in patients with hyperglycemia in the emergency department. BMC Emerg Med. 2016 Jan 29;16:7. doi: 10.1186/s12873-016-0072-7.
15. Soleimanpour H, Taghizadieh A, Niafar M, Rahmani F, Golzari SE, Esfanjani RM. Predictive value of capnography for suspected diabetic ketoacidosis in the emergency department. West J Emerg Med. 2013;14(6):590–4.
16. Fearon DM, Steele DW. End-tidal carbon dioxide predicts the presence and severity of acidosis in children with diabetes. Acad Emerg Med. 2002;9(12):1373–8.
17. Guerra, W. F., Mayfield, T. R., Meyers, M. S., Clouatre, A. E., & Riccio, J. C. (2013). Early detection and treatment of patients with severe sepsis by prehospital personnel. The Journal of emergency medicine, 44(6), 1116-1125.)
18. Hunter CL, Silvestri S, Dean M, Falk JL, Papa L. End-tidal carbon dioxide is associated with mortality and lactate in patients with suspected sepsis. American Journal of Emergency Medicine. 2013 Jan; 31(1):64-71.
19. Hunter CL, Silvestri S, Ralls R, Stone A, Walker A, Papa L. A prehospital screening tool utilizing end-tidal carbon dioxide predicts sepsis and severe sepsis. American Journal of Emergency Medicine. 2016 May; 34(5):813-819.
20. Yamanaka MK, Sue DY. Comparison of arterial-end-tidal Pco2 difference and dead space/tidal volume ratio in respiratory failure. Chest. 1987;92:832-835.
21. Hardman JG, Aitkenhead AR. Estimating alveolar dead space from the arterial to end-tidal CO2 gradient: a modeling analysis. Anesth Analg. 2003;97:1846-1851.
Additional articles of Interest:
EMS One: 5 Things to Know About Capnography in Cardiac Arrest



