A Case

It is a typical day in the emergency department. An 83 yo female is brought in by EMS after family called 911 because the patient was not herself. The patient’s vital signs are reportedly within normal limits, so she is triaged to a regular room in the emergency department where handoff is given from paramedic to nurse. The physician, who is in another room, is not present for the signout. Ten minutes later, the physician walks into the room to see the patient. Her family is not present. Because paramedics had to leave rapidly for another call, the prehospital patient-care record is not in the chart and there is minimal documentation of what was communicated in the handoff. The patient, who is oriented only to self, states only, “I’m not sure why I’m here.” The physician continues with his physical exam, hoping he can find other clues as to why the patient is here.
A couple weeks ago, we asked our readers to consider this case and discuss the following questions:
What are some of the barriers you have encountered to quality patient handoffs from prehospital to in-hospital providers ?
Most importantly, what initiatives has your EMS system implemented to address this issue in patient care?
Below you will find a summary of this discussion.
Discussion Summary
Handoffs are defined as the transfer of information, professional responsibility and accountability between caregivers. Whenever they occur, handoffs are a critical component of quality patient care and have enormous influence on patient trajectory within the clinical environment. Failures of communication during transfer of patient care are major drivers of error and patient harm within the current healthcare system [1,2].
For a multitude of reasons, handoffs between prehospital and in-hospital clinicians are logistically difficult and vary in quality. A quantitative analysis of the content of 90 EMS to ED handoffs involving critically ill patients found significant deficiencies in information transfer [3]. Only 78% (95% CI, 70.0-86.7) of handoffs included a chief concern, 47%(95% CI 31.3 – 57) included pertinent physical exam findings, and 58% (95% CI 47.7 – 67.7) provided a description of the scene. The reason for such omissions is likely multi-factorial. A qualitative study of EMS provider focus group-based discussions of handoffs identified some common themes [4]. EMS providers expressed frustration with a disorganized process that inhibited their ability to act as patient advocates. Disorganization was predominantly due to lack of time, focus, standardization, and respect for the healthcare role of the EMS provider. When asked to comment on “barriers to quality handoffs”, our readers focused on these themes as well:
“Bedside handover needs to be distinct from moving the patient to the bed. Singular focus.”
“Triage nurses (or whoever) must be on the same page as EMS with a standardized, mutually agreeable, report format.
Instead, everyone is doing their own thing and there is no consistency.
As a medic, in one shift I can effectively go from “name, date of birth,and complaint—don’t tell me anything else” to “why aren’t you giving me a full report?”
Tell me what you want and I’ll work with you!
But if you don’t want any information, you won’t have it later”
Interruptions are the norm in the chaotic environment of the emergency department. In one study, emergency physicians were interrupted 9.7 times per hour and spent 6.4 minutes out of every hour performing simultaneous tasks [5]. Following such interruptions, emergency physicians failed to return to a significant percentage (19%) of tasks. In one study of emergency department communication, 30.1% of communication events were found to be interruptive and 10% of communication time involved two or more concurrent conversations [6]. Interruption is the cultural and operational norm of the emergency department, including during times of information transfer. This undoubtedly leads to information loss and negatively impacts patient care. The question remains: how do we fix it?
One of the major themes that emerged from our reader’s comments was that of standardization:
“I think a standard handover tool between EMS and hospital providers is essential and helps ensure that just the important information that both parties are interested in are transmitted”
“Multi-provider and multi-hospital systems are complicated—everyone needs to work together. Standard handover tools are good but need to be standard and work for both EMS and ED. EMS needs to be educated as to the failures in their current methods.”
“Here in Holland all (para)medics are also RN’s (specialized in ER/ED and/or ICU) so that helps to be on the same page. With the handoff the ER doc is always present (or at least should be) and we use the SBARR method ( Situation, Background/pt Hx, Assessment, Results of treatment given, Recommendation) for all patients that we bring to the ED in the handoff and a full report we send by Ipad. ”
Indeed, in a joint statement, NAEMSP, the American College of Emergency Physicians (ACEP), Emergency Nurses Association (ENA), National Association of Emergency Medical Technicians (NAEMT) and the National Association of State EMS Officials (NAEMSO) wrote that a “clearly defined processes for the contemporaneous face-to-face communication of key information from … EMS providers to health care providers in an emergency department are critical to improving patient safety, reducing medicolegal risk, and integrating EMS with the healthcare system.” [7]. But is standardization of the handoff process effective in improving the quality of information transfer?
In 2007, a study was published that evaluated the effect of implementing a standardized tool on retention of information by ED staff following EMS handoffs [8]. The study measured information recall by the ED staff during unstructured handoffs versus handoffs structured in the “DeMIST” format: Demographics, Mechanism of injury/illness, Injuries (sustained and suspected), Signs (including observation and monitoring), and Treatment given. Overall, they reported a non-significant decrease in information retained after implementation of the standardization tool (from 56.6 to 49.2%), which is disheartening until the study is evaluated more closely. First, only EMS providers were trained in the format, and this training was minimal. Second, only 18 unstructured handoffs and 10 structure handoffs were evaluated. Therefore, the take-home of this study is not that standardization is ineffective, but that simply changing the format of the handover, rather than the process of the entire system (EMS and ED) is ineffective in creating change.
On the hospital side, there is some evidence that standardization of information transfer can be effective in improving patient-centered outcomes. A very large study of the effect of implementing a standardized handoff tool for pediatrics residents (I-PASS) found a 23% decrease in the medical-error rate in 10,740 patient admissions [2]. Importantly, the intervention was not limited to the mnemonic itself, but included extensive education, resident feedback, and a culture-change campaign.
One of our readers commented specifically on a local initiative in standardization:
“The regional EMS council encompassing Rochester, NY implemented [a standardized handoff process] last year. While not universally utilized (on either side of the transition), when it is the transfer of care is noticeably smoother”
Source: https://www.mlrems.org/patient-handoff/ems-toolkit/
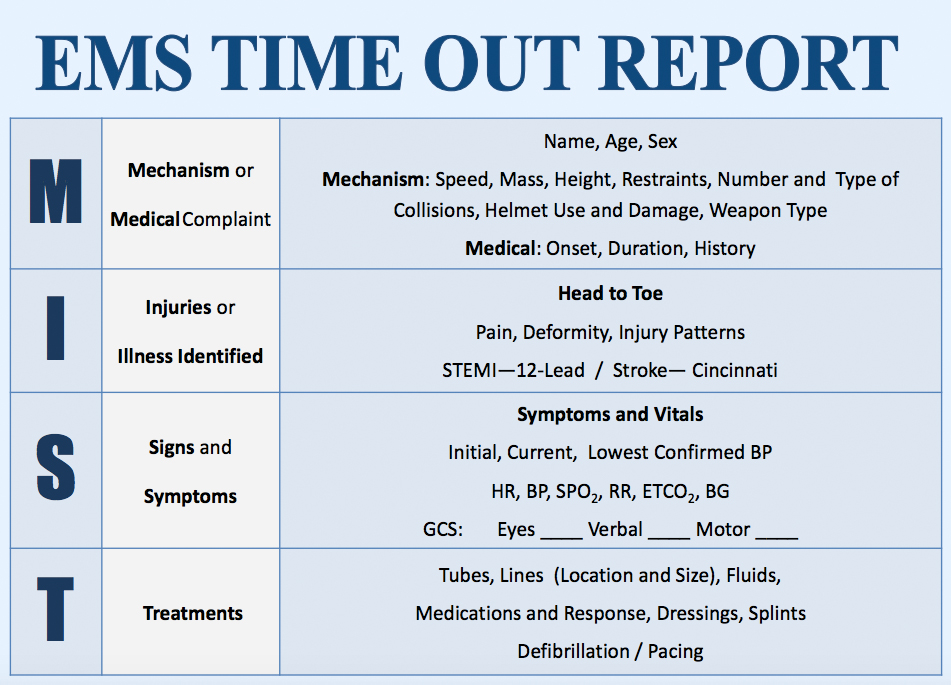
The Monroe-Livingston Region in upstate New York enacted a program entitled “Effective Patient Handoffs”. This program employs a standardized MIST handoff tool for the transfer of information (see Figure). Moreover, it requires that information transfer is the singular focus of the interaction (i.e. occurs prior to and not simultaneously with movement of the patient). It is not a unilateral initiative, but elicited the collaboration of emergency departments in the area. Educational videos and posters are provided on the website. Based on the I-PASS study, such tools are essential to creating the cultural change to enable effective implementation.
But verbal communication is only part of the communication between EMS and the ED. As noted by the joint statement by NAEMSP, ACEP, ENA, NAEMT and NAEMSO, “verbal information alone may lead to inaccurate and incomplete documentation of information and inadequate availability of information to subsequent treating providers… who are not present at the verbal communication.” [7]. Indeed, the study of the DeMIST handoff tool reinforced this concept by demonstrating that only about half of information is retained following the verbal transfer of information [8]. Several of the comments addressed the importance of written documentation during transfer of information:
“I think a good triage note from the RN taking the bedside is also important when the physician is unable to talk to EMS. With EHRs the ability to standardize this and ensure that pertinent EMS information is documented directly in the patient’s chart is fairly simple.”
“…and a full report we send by Ipad. ”
“The runsheet needs to be valued by both EMS and ED. Completed and submitted to the server in a short period of time. ”
EMS documentation is part of the healthcare record, but counter to this fact, many EMRs fail to integrate prehospital information into the patient’s permanent care record. Beyond written documentation of the handoff by the direct receiver (triage note), the EMS patient care record, including prehospital testing such as glucose measurement and ECG, are often unavailable within a clinically relevant period of time. While most electronic records are designed to capture billing information, we must remain vigilant that they effectively perform what should be their primary role – efficient transfer of information for patient benefit. While we wait for technology to catch up (as it has in other parts of the world such as Holland per our reader’s comments), we must remain consistent in recognizing the value of prehospital written documentation.
Take Home
The handoff between EMS and the ED is a critical moment in patient care. As clinicians working in the prehospital environment, emergency department or both, we must change both the process and culture surrounding verbal and written documentation if we are to do the best for our patients.
If you read this article, please consider completing the following survey:
Discussion summary by EMS MEd Editor, Maia Dorsett MD Phd (@maiadorsett)
References
1. Joint Commission. (2016). Sentinel event data: root causes by event type, 2004–2015. PowerPoint slides, Retrieved from the Joint Commission website) http://www. jointcommission. org/sentinel_event. aspx.
2. Starmer, A. J., Spector, N. D., Srivastava, R., West, D. C., Rosenbluth, G., Allen, A. D., … & Lipsitz, S. R. (2014). Changes in medical errors after implementation of a handoff program. New England Journal of Medicine, 371(19), 1803-1812.
3. Goldberg, S. A., Porat, A., Strother, C. G., Lim, N. Q., Wijeratne, H. S., Sanchez, G., & Munjal, K. G. (2017). Quantitative analysis of the content of EMS handoff of critically ill and injured patients to the emergency department. Prehospital Emergency Care, 21(1), 14-17.
4. Meisel, Z. F., Shea, J. A., Peacock, N. J., Dickinson, E. T., Paciotti, B., Bhatia, R., … & Cannuscio, C. C. (2015). Optimizing the patient handoff between emergency medical services and the emergency department. Annals of emergency medicine, 65(3), 310-317.
5. Laxmisan, A., Hakimzada, F., Sayan, O. R., Green, R. A., Zhang, J., & Patel, V. L. (2007). The multitasking clinician: decision-making and cognitive demand during and after team handoffs in emergency care. International journal of medical informatics, 76(11), 801-811.
6. Coiera, E. W., Jayasuriya, R. A., Hardy, J., Bannan, A., & Thorpe, M. E. (2002). Communication loads on clinical staff in the emergency department. The Medical Journal of Australia, 176(9), 415-418.
7. American College of Emergency Physicians, Emergency Nurses Association, National Association of EMS Physicians, & National Association of State EMS Officials. (2014). Transfer of patient care between EMS providers and receiving facilities. Prehospital emergency care: official journal of the National Association of EMS Physicians and the National Association of State EMS Directors, 18(2), 305.
8. Talbot, R., & Bleetman, A. (2007). Retention of information by emergency department staff at ambulance handover: do standardised approaches work?. Emergency Medicine Journal, 24(8), 539-542.



