Prehospital Plasma during Air Medical Transport in Trauma Patients at Risk for Hemorrhagic Shock
Background & Objectives:
Hemorrhagic shock remains the most significant cause of mortality in trauma patients. In particular, coagulopathy is a significant contributor to death in this patient population and has been a focus of what is termed “damage-control resuscitation” in both civilian and battlefield arenas. Currently, there is a stronger push for resuscitation with blood-components including platelets and packed red cells in favor over crystalloid based resuscitation strategies. The premise of early damage control resuscitation in the pre-hospital environment is predicated on intervening at the point of injury and mitigating downstream complications including coagulopathy and irreversible hemorrhagic shock. Plasma administration as part of damage control resuscitation is thought directly address coagulopathy and improve chances for survival. This trial, termed the “Prehospital Air Medical Plasma (PAMPer)” trial sought to investigate the efficacy and safety of prehospital plasma administration in severely injured trauma patients. The primary outcome was the impact of prehospital plasma administration on 30 day mortality.
Methods:
The investigators conducted a phase 3 multi-center cluster-randomized trial involving trauma patients (blunt or penetrating) who were deemed to be at risk for hemorrhagic shock during air medical transport. Individual air medical bases were randomized to give plasma vs standard resuscitation in 1 month blocks. The intervention arm included patients who received 2 units of universal donor thawed plasma. The comparison group received standard of care resuscitation (crystalloid based resuscitation). Patients were deemed to be “at risk” for hemorrhagic shock were enrolled in the trial if they had at least one episode of hypotension (defined as systolic BP <90 mm Hg) and tachycardia (defined as HR >108 BPM) or if they had severe hypotension (defined as SBP <70 mm Hg) at any point in the prehospital phase of care. There were several exclusion criteria some of which included patients older than age 90 or younger than age 18, individuals who were pregnant, had traumatic cardiac arrest lasting longer than 5 minutes, penetrating brain injury, or refusal by family member to participate in the trial or if the patient was wearing an “opt-out” bracelet reflecting their wish not to participate in the trial, among others.
Key Results:
There were 27 air medical transport bases that were recruited for the study that transported patients to 9 different level 1 trauma centers across the United States between 2014 to 2017. In total, 7,275 patients were transported during the study period, of which 501 patients qualified for the study. Of these patients, 230 received plasma and 271 received standard care resuscitation. Average prehospital time was 40 minutes (95% CI 33-51) and 42 minutes (95% CI 34 to 53) in the plasma and saline treated groups respectively. The key findings were as follows:
-
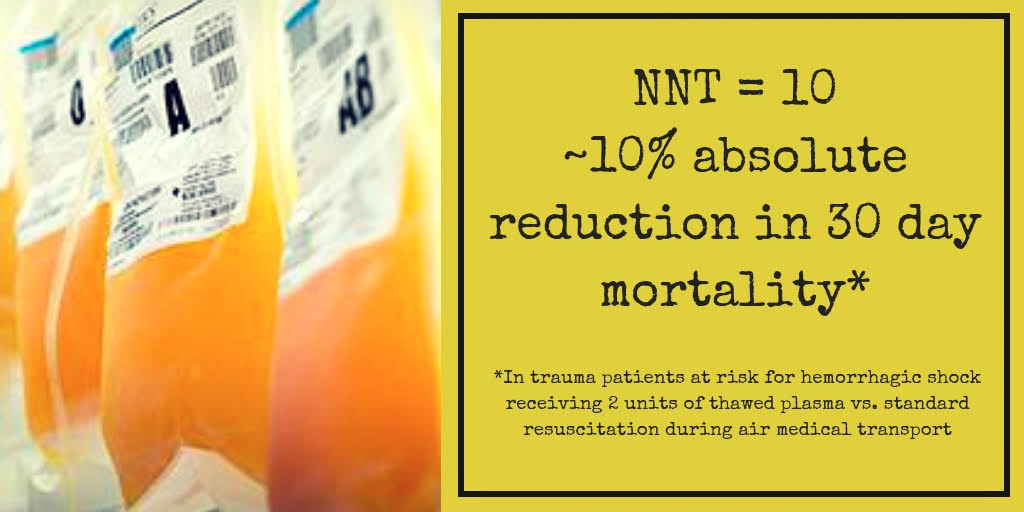
Mortality at 30 days was significantly lower in the plasma group (23.2%) versus standard group (33.0%)
-
Absolute reduction was 9.8% in the plasma group (95% CI 1.0 to 18.6%; P=0.03).
-
Median INR was lower in plasma group compared to standard group (1.2 vs 1.3; p<0.001)
-
No statistically significant difference was found in secondary outcomes including 24-hr mortality, in-hospital mortality, volume of pRBC transfusion in the first 24 hrs, multi-organ failure, acute lung injury/ARDS, or transfusion-related reactions after correction for multiple comparisons.
-
Number needed to treat (NNT) was 10.
Takeaways:
-
In this prospective trial administration of plasma in the prehospital aeromedical transport setting was associated with decreased 30 day mortality in trauma patients at risk for hemorrhagic shock.
What this means for EMS:
In 2015, the PROPPR trial demonstrated improved outcomes in trauma patients receiving blood products (packed red cells, platelets, plasma) compared to crystalloid resuscitation. Little research has been done on the role of plasma administration at the point of injury in the prehospital setting. This study was one of the first to show that rapid prehospital administration of plasma products is associated with improved 30 day mortality. As stated in Article Bite #4, transfusion of blood products in the prehospital setting is associated with many logistical roadblocks, including but not limited to a refrigeration, coordination with blood banks, and issues pertaining to wastage of products with a short shelf life, are all important considerations prior to routine implementation of this intervention. Given the traditional model of prehospital trauma care has focused on rapid transfer to a trauma center for definitive management, prehospital administration of plasma is a potential intervention that may lead to improved patient outcomes in some systems where distance to trauma center leads to extended prehospital times*.
Article summary and figure by Article Bites Editor Al Lulla, MD
* The COMBAT trial, which evaluated prehospital plasma transfusion for patients with signs of hemorrhagic shock within an urban system, did not find similar benefit.