A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest
Background & Objectives:
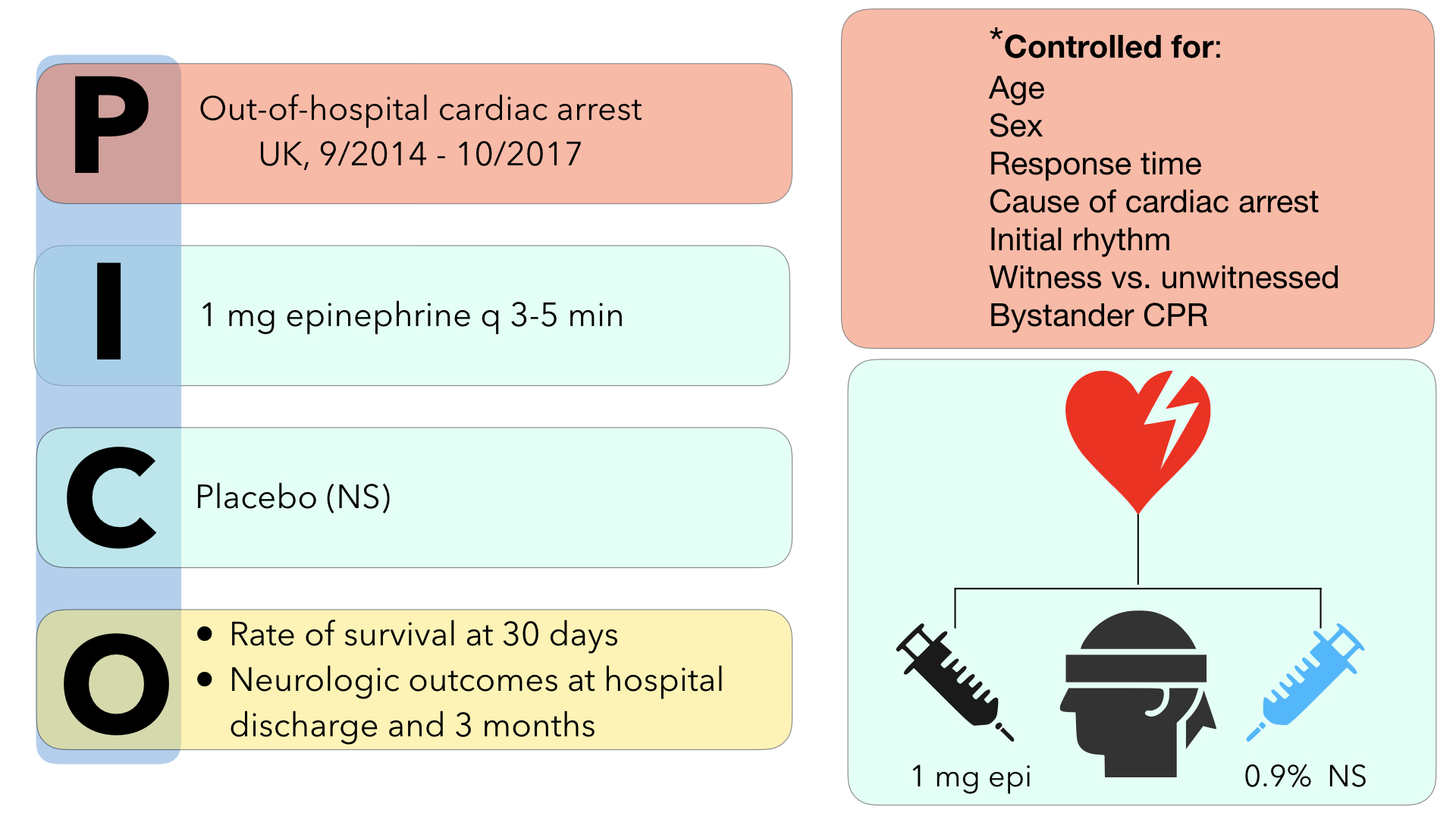
Other than early CPR and defibrillation, there are few measures that have been shown to improve outcomes for out-of-hospital cardiac arrest (OHCA). Despite this, epinephrine has been at the crux of ACLS management of patients with OHCA given the thought that it can cause peripheral vasoconstriction, increased beta adrenergic activity and augment coronary blood flow. In turn, epinephrine increase chances of return of spontaneous circulation (ROSC). While higher rates of ROSC have been confirmed in prior studies on epinephrine, unfortunately most of what we know about epinephrine suggests that it’s administration may not improve the most important clinical outcome – neurologically intact survival. The PARAMEDIC2 trial (Prehospital Assessment of the Role of Adrenaline: Measuring the Effectiveness of Drug Administration in Cardiac Arrest) was performed to assess whether epinephrine was beneficial or harmful as demonstrated by the primary outcome of 30 day survival.
Methods:
The investigators conducted a multi agency (5 ambulance services), randomized, double-blind, placebo controlled trial in the United Kingdom from December 2014 to October 2017 in adult patients who sustained OHCA for which ACLS was provided by paramedics. Patients were excluded from the trial if they were pregnant, less than 16 years of age, had cardiac arrest secondary to anaphylaxis or asthma, or if they had administration of epinephrine prior to the arrival of EMS personnel. If initial resuscitation measures (CPR and defibrillation) were unsuccessful, patients were randomized to the intervention arm (1mg epinephrine q3-5 mins in accordance with ACLS protocols) or the control arm (normal saline placebo). As stated above, the primary outcome of the trial was 30 day survival. Secondary outcomes that were examined included rate of survival until hospital admission, length of hospital stay and ICU stay, rates of survival at hospital discharge and at 3 months, neurological outcomes at hospital discharge and at 3 months. Favorable neurological outcome was defined as modified Ranking score of 3 or less.
Key Results:
In total, 8014 patients with OHCA were enrolled in the study over the 3 year period of which 4015 patients were in the intervention arm (epinephrine) compared to 3999 patients in the placebo arm. Both groups were well matched in terms of baseline patient characteristics.The key results from the trial were as follows:
-
30 day survival: 3.2% in epinephrine group vs 2.4% in placebo group (OR 1.39; 95% CI 1.06-1.82, p=0.02).
-
Favorable neurological survival at 3 months (modified Rankin score 3 or less): 2.1% in epinephrine group vs. 1.6% in placebo group (OR 1.31; 95% CI 0.94-1.82.
-
Severe neurological impairment (modified Rankin score 4 or 5): 31% in epinephrine group vs. 17.8% in placebo group
-
ROSC during prehospital resuscitation: 36.3% in epinephrine group vs. 11.7% in placebo group
Takeaways:In this multi-agency, prospective, double blinded randomized placebo controlled trial, administration of epinephrine for OHCA was associated with a statistically significant higher 30 day rate of survival compared to placebo, but no difference in neurologically-intact survival.
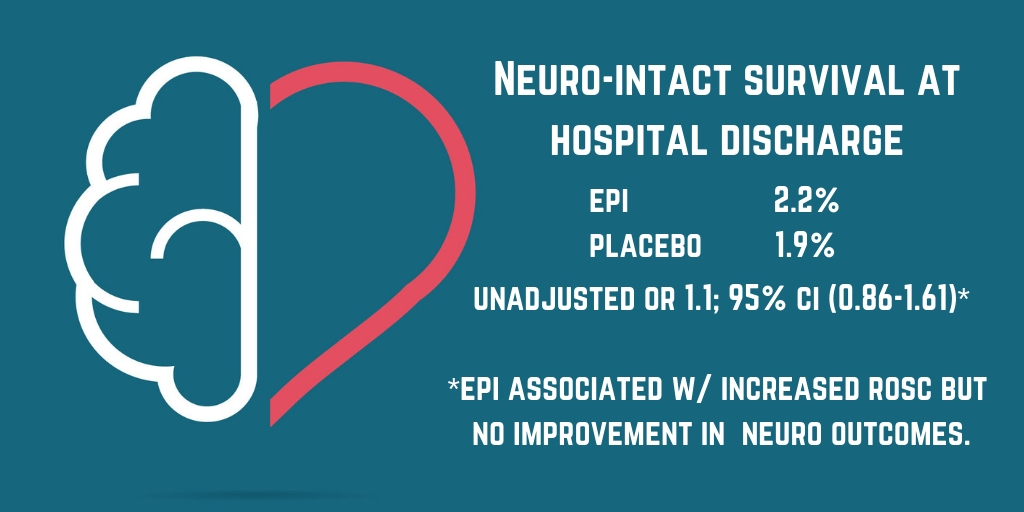
What this means for EMS:This study is the largest randomized controlled trial performed to date studying the impact of epinephrine administration on survival and neurological outcomes for OHCA. While administration of epinephrine has long been the pharmacological mainstay of prehospital (as well as in-hospital) management of OHCA, this trial calls into question its influence on patient centered outcomes (i.e. neurological intact survival). While this paper will surely be at the center of debate in the upcoming years within EMS circles around the world, one thing remains abundantly clear at this point: good quality BLS Care in the form high quality CPR and early defibrillation have the greatest impact on neurologically intact survival and should be the primary focus of resuscitation for cardiac arrest.