Analysis of Out-of-Hospital Pediatric Intubation by an Australian Helicopter Emergency Medical Service.
Background & Objectives:
Adequate establishment and maintenance of a patent airway is one of the hallmarks of resuscitation. Pediatric intubation poses particular challenges, most notably lack of provider experience. It is estimated that first-pass success ranges from 66% to 85%. Prior studies have demonstrated no significant improvement in pediatric outcomes with prehospital intubation. The intubation success rate in this study was only 57%. [1] Despite the difficulties associated with pediatric intubation, it remains within the scope of practice in the prehospital setting in some EMS services. The primary goal of this study was to report first-look success rate in pediatric advanced airway management in a physician-led adult out-of-hospital helicopter retrieval service. The secondary goal was to evaluate for potential complications of airway management as well as success by operator type, patient age and type of intubation.
Methods:
The investigators conducted a retrospective study evaluating patients who were treated by the Greater Sydney Area Helicopter Emergency Medical Service in Australia. This helicopter EMS service (HEMS) is comprised of a 2-person medical team with a physician and a paramedic. Physicians were usually board certified in emergency medicine or anesthesiology or residents with at least 5 years of experience. Paramedics were critical care paramedics with 10 years of experience and additional training with out of hospital care and retrieval medicine. The investigators evaluated an analysis of all out of hospital and interhospital pediatric intubations between January 2010 and April 2015. The only inclusion criteria was that the patient be younger than 16 years of age. Patients were intubated at the discretion of the team, with rapid sequence intubation (RSI) versus cold intubation (most frequently for cardiac arrest). The measures that were reported included critical timings (i.e. time to intubation), demographics, provider background, number of intubation attempts and complications.
Key Results:
In total there were 10,856 patients treated during the study period, of which 497 (4.6%) were pediatric patients. Of these patients, 82 (16.5%) were intubated by this particular HEMS service. The key findings were as follows:
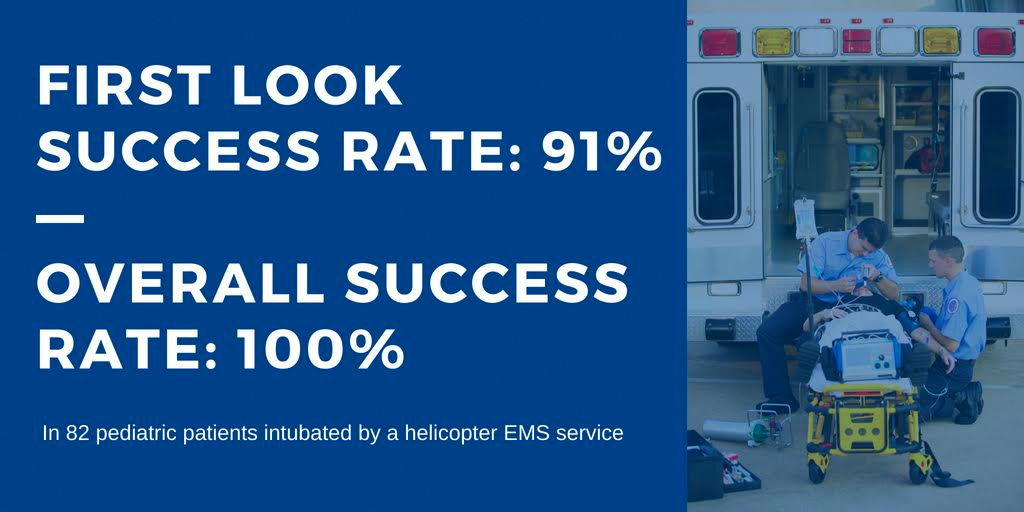
- First look success rate: 91% (75/82; 95% CI 83 to 97%). The overall success rate was 100%.
- 80% of patients were successfully intubated within 1 to 2 minutes after induction
- 69/82 (84%) were rapid sequence inductions (RSI)
- Ketamine was the most commonly used induction agent, utilized in 63/69 patients (91%) undergoing RSI
- The most common indications for intubation included trauma (83%), head injury (56%), combative/agitated patient (29%).
- Median time to intubation was 25 minutes (defined as time from HEMS arrival to intubation)
- Complication rate including hypotension, bradycardia and desaturation was 14%
- Difficult airway indicators were present in 77% of patients that were intubated by this service
Takeaways:
- In this retrospective series of pediatric intubations in the prehospital setting by a physician-lead helicopter service, first pass success was 91%. Overall success rate was 100% with only 9% of patients requiring multiple attempts).
What this means for EMS:
The role of intubation in the field for pediatric patients is extremely controversial. Prior studies have demonstrated low rates of first pass success and overall lack of significant improvement in patient outcomes. This study showed an uncharacteristically high rate of first past success in the prehospital setting for pediatric patients. The investigators of this study attribute their high rate of success to a rigorous training program for providers in the field, frequent practice and checklists amongst other mandated practices. Overall, pediatric intubation in the field is a relatively rare occurrence with limited “on-the-job” training experience, which may be what has historically contributed to its unsuccessful implementation in the field. This study highlights the importance of adequate training and psychomotor mastery to performance of critical skills, particularly those that are rarely performed. It did not evaluate the effect on clinical outcomes.
References:
1. Gausche, M., Lewis, R. J., Stratton, S. J., Haynes, B. E., Gunter, C. S., Goodrich, S. M., … & Seidel, J. S. (2000). Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. Jama, 283(6), 783-790.