by Aaron Farney, MD
Case Presentation
EMS is dispatched priority 1 for an 86-year-old female unconscious/fainting call. Despite 911 center implementation of the Medical Priority Dispatch System (MPDS) 36 pandemic card, this incident is coded via the 31 card – unconscious/fainting.
On arrival, EMS discovers family in an upstairs bathroom surrounding an elderly female who is weak and has fallen off the toilet after defecating. Family reports they were nearby, saw her start to faint and helped her down to the floor. She reportedly did not strike her head or completely lose consciousness. The patient has been experiencing diarrhea for approximately five days, has had decreased fluid intake, and worsening generalized weakness culminating in a fall. She denies chest pain. Family confirms the patient is full code.
Her medical history is most pertinent for diabetes mellitus, high blood pressure, and coronary artery disease with a prior myocardial infarction. Medications are most notable for aspirin, insulin, torsemide and supplemental potassium. She does not take anticoagulants. She has continued to take her medications throughout her present illness.
On exam, the patient is alert but confused, able to follow commands, with a small contusion over her forehead. She is ill-appearing and partially covered in stool. Heart rate is 120 and irregular, blood pressure is 128/67, she is breathing 30 respirations/minutes, and room air pulse oximetry is 87%. She appears to be in respiratory distress with poor perfusion.
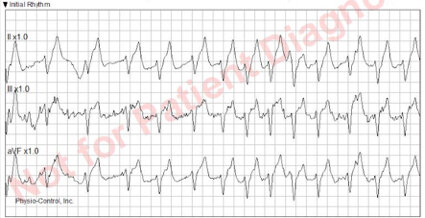
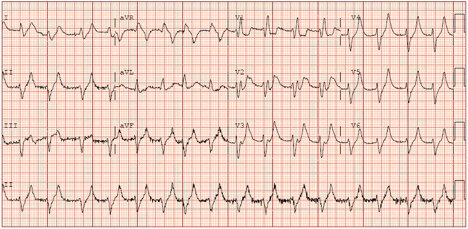
Initial rhythm strip is below:
EMS 12 lead EKG is below:
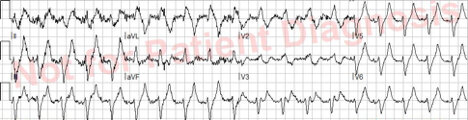
EMS applies supplemental oxygen via a non-rebreather mask, grossly decontaminates her, and rapidly moves her to the stretcher via a patient mover tarp and stairchair. Transport is commenced to the nearest STEMI center. Enroute, vascular access is established, an IV fluid bolus is initiated, and the receiving hospital is notified of an inbound potential STEMI candidate. Blood glucose is 300.
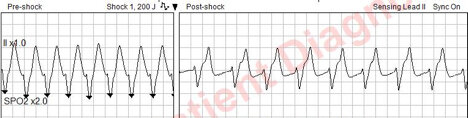
While enroute, the patient suddenly loses consciousness and the paramedic notes a change in rhythm. A synchronized shock is delivered at 200 J, resulting in successful cardioversion as seen below.
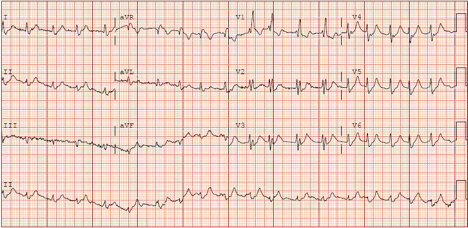
On arrival at the hospital, EMS is met by the Emergency Medicine and cath lab team. Initial hospital EKG is below.
The STEMI alert is called off and intravenous calcium is administered while laboratories are pending. A repeat EKG following calcium administration is below:
The patient is further stabilized with intravenous insulin/dextrose, sodium bicarbonate, IV fluids, furosemide, and antibiotics. A foley catheter is inserted and no urine output is observed. Nephrology is emergently consulted while labs are pending. Potassium returns at 8.3. The patient is admitted to the ICU. A COVID-19 swab is sent off and subsequently results positive.
Case Summary
This is a case of a patient presenting with a substantially abnormal EKG mimicking a STEMI, associated with electrical instability & multiple runs of wide complex tachycardia, ultimately found to have hyperkalemia. The hyperkalemia is likely secondary to acute renal failure, in turn caused by severe dehydration secondary to diarrhea from COVID-19 infection, complicated by continued compliance with diuretic medication and potassium supplementation.
The history and EKG are highly suggestive of hyperkalemia and warranted emergent empiric treatment with IV calcium. Rapid administration of intravenous calcium is a life-saving intervention that immediately shields the cardiac myocytes from the effects of potassium, mitigating electrical disturbances seen in severe hyperkalemia. IV calcium can be administered prehospital, either by standing order when applicable, or by consultation with online medical control. The impact is realized very quickly, as evidenced by the repeat EKG demonstrated above following calcium administration.
EMS took all appropriate PPE precautions throughout this incident.
Take Home Points
· Hyperkalemia can be seen in patients with no prior history of renal disease
· Diarrhea is a known cause of dehydration and acute renal failure than can cause electrolyte disturbances
· Severe hyperkalemia causes a variety of EKG changes, including peaked T waves and widened QRS complexes that may mimic a STEMI
· Patients with EKG changes from hyperkalemia warrant IV calcium administration
· COVID-19 can present in a variety of chief complaints and symptoms, and may manifest in odd ways due to downstream impact on end organ systems
· It is imperative that EMS remains vigilant and exercises a high degree of suspicion for COVID-19