by Kaitlyn Hartnett, MS2 NRP and Joshua Stilley, MD FAEMS
Case:
You are dispatched to a 60 year old female with a chief complaint of dizziness. Upon arrival, the patient is lying on her bed in a dark room, but is interactive. Vital signs are normal, and her primary survey is unremarkable. She tells you that approximately 2 hours prior she “began feeling continuously dizzy and everything is spinning hard to the left.” The patient informs you that every time she opens her eyes or tries to stand, she vomits and falls to the floor due to the spinning. Her stroke exam (LAPSS and/or CPSS) is negative, and glucose is 110. Upon moving the patient, she begins vomiting continuously and requires significant support on her left side to keep her upright. Further examination reveals photosensitivity and non-fatigable, horizontal nystagmus. You are concerned for a stroke, but your stroke scales were negative.
Cognitive detour:
Having confidence in a decision is not the same thing as having competence in a decision. I am sure we have all met someone in the public safety or healthcare world that was sure they had all of the answers, but everyone else was aware they did not. It is just as likely that we all at times are overconfident in a decision for which we do not have the competence to make. Drs Justin Kruger and David Dunning published a paper in 1999 that has been widely cited, and their observation is called the Dunning-Kruger effect. [1] The cognitive error comes not from the lack of competence, but the lack of the awareness of the lack of competence – i.e. not knowing what you don’t know. People have the erroneous impression they are doing just fine.
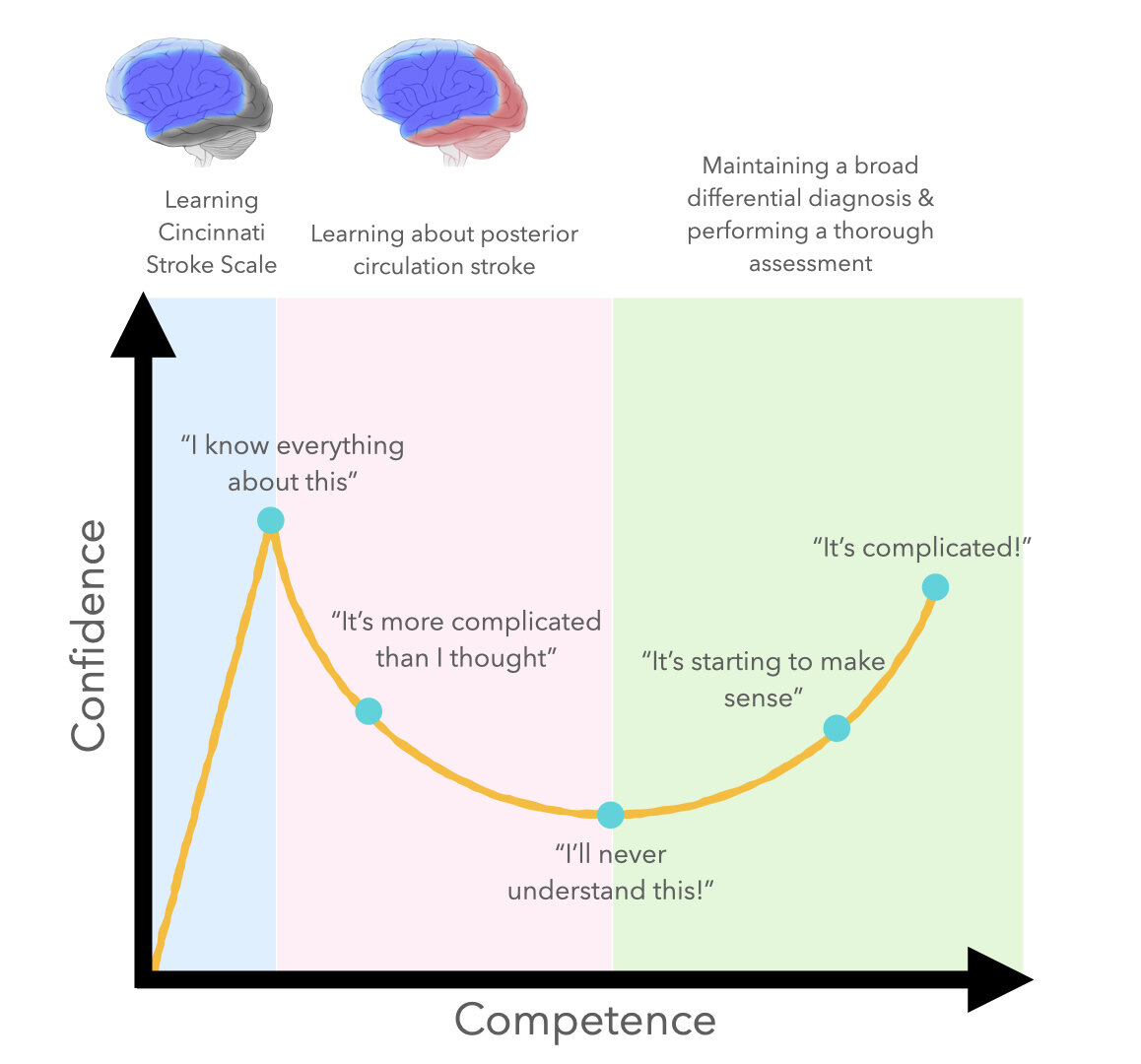
Figure: The Dunning-Kruger curve for stroke assessment
An interesting example Dr. Dunning gave as a lightbulb moment for their research is a suspect arrested after a bank robbery. [2] The suspect stated that because he put lemon juice on his face, he thought the cameras would not be able to identify him. When questioned further, he stated he tested it with a polaroid camera prior to the robbery attempt. Since the photo came out blurry, it confirmed the theory. Dr. Dunning realized the possibility that not only was the robber too unintelligent to be a bank robber, he was also too ignorant to know that he was too unintelligent to be a bank robber.
A novice should know they are a novice; there is no need to inform them that they cannot complete a task at a high level. Overconfidence at this point can be a detriment to patient care, as we are unaware of what we do not know and subsequently think in terms of definitive yes/no answers (Figure)… i.e. negative CPSS = patient is not having a stroke. As we gain more knowledge, we become aware of all that we do not know and tend to develop a lack of confidence as we realize our own ignorance. This can come in the course of education or often in the context of a real clinical case where we realize that we missed something or made a mistake. This can be overwhelming, but the road to expertise relies on grasping on to this as a motivator to learn more, seek feedback and elevate the level of care that we provide by actively looking for and addressing gaps in our knowledge.
Back to the Case
A cerebellar stroke is one of the more difficult diagnoses to make clinically. There can be a lot of symptomatic overlap between a cerebellar stroke and benign causes of vertigo (not to mention intoxication). Two big keys that should prompt a consideration for cerebellar stroke include sudden onset, symptoms that happen without though may be exacerbated by head or body movement, and ataxia. Dizziness has a broad differential and this chief complaint should prompt consideration and assessment for stroke beyond the Cincinnati stroke scale. The inability to coordinate muscle movement should be very concerning for cerebellar involvement, as the cerebellum is the brain’s coordination center. Patients with peripheral vertigo are often reluctant to walk due to discomfort, but are typically able to ambulate independently.
Patterns of nystagmus can also be used to help differentiate causes of vertigo.[3,4] Nystagmus caused by peripheral pathology is generally fatigable and strongly associated with positional induction of horizontal nystagmus. Nystagmus caused by central pathology, on the other hand, is often non-fatigable and can present with a combination of horizontal, vertical, or torsional nystagmus. The presence of vertical or torsional nystagmus is highly suggestive of a central origin of vertigo, however, the absence of this eye pattern does not rule out a central cause.
Because the aforementioned patient was unable to sit or walk without substantial assistance, there should be an immediate concern for a central cause of vertigo. Additionally, the presence of non-fatigable nystagmus, even in the absence of vertical or torsional direction, further supports a central origin. At this point, you should be concerned that the patient is experiencing a cerebellar stroke necessitating time sensitive intervention, prompting transport to a stroke center and a stroke alert activation.
References:
1. Kruger J, Dunning D. Unskilled and unaware of it: how difficulties in recognizing one\’s own incompetence lead to inflated self-assessments. J Pers Soc Psychol. 1999 Dec;77(6):1121-34. doi: 10.1037//0022-3514.77.6.1121. PMID: 10626367.
2. Morris, Errol. The Anosognosic’s Dilemma: Something’s Wrong but You’ll Never Know What It Is (Part 1). New York Times Blog. 2010. https://opinionator.blogs.nytimes.com/2010/06/20/the-anosognosics-dilemma-1/
3. Nelson JA, Viirre E. The clinical differentiation of cerebellar infarction from common vertigo syndromes. West J Emerg Med. 2009 Nov;10(4):273-7. PMID: 20046249; PMCID: PMC2791733.
4. Edlow JA, Gurley KL, Newman-Toker DE. A New Diagnostic Approach to the Adult Patient with Acute Dizziness. J Emerg Med. 2018 Apr;54(4):469-483. doi: 10.1016/j.jemermed.2017.12.024. Epub 2018 Feb 1. PMID: 29395695; PMCID: PMC6049818.
EMS MEd Editor & Image design: Maia Dorsett, MD PhD FAEMS FACEP, @maiadorsett