By Casey Patrick MD and Brad Ward EMT-P
Article: E Baldi, S Schnaubelt, et al. Post-ROSC electrocardiogram timing in the management of out-of-hospital cardiac arrest: results of an international multicentric study (PEACE study). European Heart Journal, Volume 41, November 2020
Background
The initial hospital destination for OHCA patients, post-ROSC, has been a moving target over the past few years. Initial retrospective data suggested that “likely cardiac source” post-arrest patients, STEMI or not, had improved outcomes with emergent cardiac catheterization (1). However, the prospective and randomized COACT study showed no benefit for emergent revascularization in non-STEMI/post-ROSC patients (2). What about those post-ROSC with STEMI? How sure are we that this group has an acute occlusion warranting emergent cath lab transport, and is there a way for better prehospital prognostication? The PEACE study set out to assist in this complex decision.
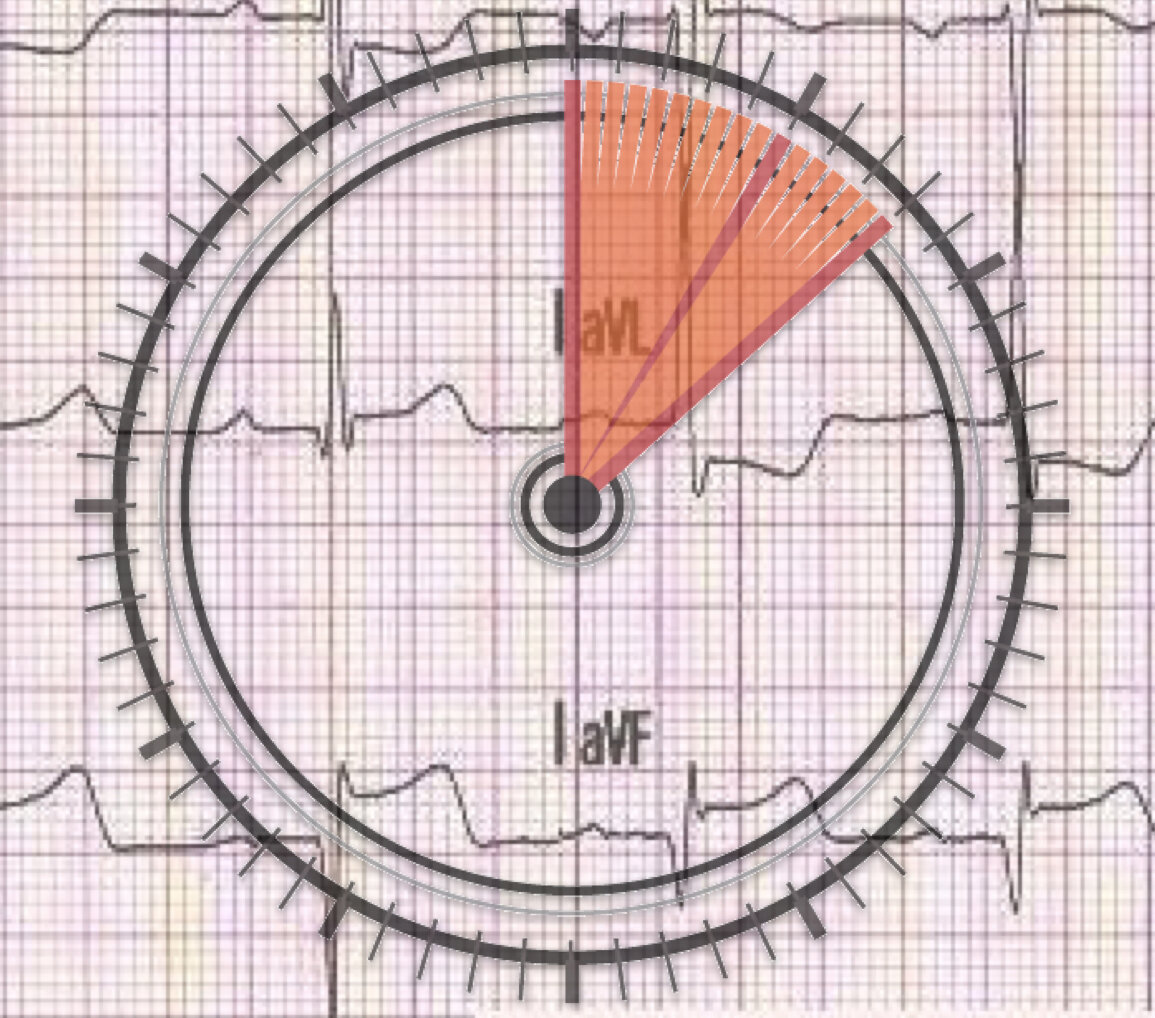
Patients who achieve ROSC after cardiac arrest are a wildly heterogeneous group with correspondingly variable courses of treatment. The 12-Lead ECG is a vital tool in our EMS diagnostic armamentarium, and we’ve taught that the sooner, the better. How soon is too soon? Does the timing of ECG capture post return of circulation affect its accuracy in diagnosing actual acute occlusive coronary disease?
Methods
This was a retrospective, cohort, multi-center study that included all OHCA patients with ECGs and eventual angiography in three European (Italy/Switzerland/Austria) hospitals from January 2015 – December 2018.
The primary outcome was false positive ECG (STEMI with no coronary obstruction). ECG’s were evaluated by two cardiologists who were blinded to all times and angiography results, and if any disagreement, a third broke the tie. Isolated posterior MI’s and Sgarbossa positive ECGs were included. Significant stenosis was defined as >50% LMCA lesion or >75% elsewhere.
All patients greater than 18yo were included with the exception of non-medical cardiac arrest causes. Five hundred eighty-six consecutive post-ROSC patients were admitted, but 152 had no ECG, and 64 did not undergo angiography. This yielded 370 patients in the final analysis.
The Results
Of the 370 patients, 198 had STEMI, and 172 did not. ~85% of patients had witnessed OHCA, with 73% receiving bystander CPR. 85% presented with an initial shockable rhythm, and 57% had good neurologic survival (defined as CPC1/2). The patients were primarily male (~75%) and in their 60’s.
How did the STEMI and non-STEMI patient groups compare? The STEMI patients were more likely initially shockable and, therefore, received more defibrillations and higher doses of epinephrine. Also, 80% of STEMI patients got PTCA vs. 57% of non-STEMI, making sense from a therapeutic momentum standpoint.
What about ECG timing? Let’s get to the good stuff and answer their question, did the timing of ECG post-ROSC change the predictive value for finding acute coronary occlusion? A logical hypothesis is yes, as earlier ECGs might be more likely false positive due to an overlap of ST-elevation from cardiac arrest ischemia/low flow (similar to type 2 MI) as opposed to signifying a true culprit lesion. The groups were stratified into ROSC-to-ECG time cohorts and then analyzed for the rate of false positives:
· 128 ECGs <8 minutes False Positive Rate = 18.5%
· 126 ECGs 8-33 minutes False Positive Rate = 7%
· 121 ECGs >33 minutes False Positive Rate = 5.8%
These differences in accuracy remained when adjusted for age, sex, epinephrine dose, defibrillation number, and pulse.
~60% improvement in ECG accuracy for actual coronary occlusion if ECG is delayed at least 8 minutes.
What Should We Do Now?
The PEACE study addressed a novel question that warrants additional investigation. On the strength side, this was a multi-center data set, but the retrospective nature is a potential source of bias. Additionally, post-ROSC ECGs were missing in 25% of patients, and angiography was not performed in a significant portion due to death before intervention.
We know that COACT and other more recent retrospective data (3) suggest immediate cath is not warranted in post-ROSC patients without STEMI. The PEACE study suggests that delaying our EMS ECG at least 8 minutes may lead to better accuracy in identifying those with acute occlusion. Should we overhaul our protocols? My opinion (take it with a grain of salt) is probably not. However, PEACE is an excellent reminder to focus on proven “lifesavers” after ROSC, and to remember that an immediate 12-lead is likely NOT one of those. Our focus should be on oxygenation, circulatory support, lung-protective ventilation, and adequate sedation. THEN…capture the ECG. Realistically, those critical steps, which we know impact mortality, should probably take 8-10 minutes anyway, so we won’t actually change as much as we’ll rearrange.
The BOTTOM LINE…
In patients with OHCA, ROSC, and subsequent angiography, the ECG was 60% more accurate for acute occlusion when delayed >8min post-ROSC. Presumably, this resulted from weeding out some ST elevation due to low flow ischemia as opposed to true obstruction. Lung protection, sedation, circulatory support, and oxygenation FIRST/ECG last – REARRANGE/DON’T CHANGE.
References:
1. Hollenbeck RD, McPherson JA, Mooney MR, Unger BT, Patel NC, McMullan PW Jr, Hsu CH, Seder DB, Kern KB. Early cardiac catheterization is associated with improved survival in comatose survivors of cardiac arrest without STEMI. Resuscitation. 2014 Jan;85(1):88-95.
2. Lemkes JS, Janssens GN, van der Hoeven NW, et al. Coronary Angiography After Cardiac Arrest Without ST-Segment Elevation. N Engl J Med 2019;380:1397-407.
3. Voicu S, Bajoras V, Gall E, Deye N, Malissin I, Dillinger JG, Benajiba C, Logeart D, Henry P, Megarbane B, Sideris G. Immediate coronary angiogram in out-of-hospital cardiac arrest patients with non-shockable initial rhythm and without ST-segment elevation – Is there a clinical benefit? Resuscitation. 2020 Oct;155:226-233.



