Article Summary by Elizabeth Stevens, MD, MA
Background:
Exertional heat stroke (EHS) is end organ dysfunction due to hyperthermia developed from physical activity. It is characterized by hyperthermia (>40.5 degrees Celsius) with end-organ dysfunction, which typically manifests as central nervous system dysfunction. Gold standard treatment of EHS is cold water immersion, which can be difficult to achieve in prehospital settings. This article summarizes the consensus of best practices for prehospital care of EHS, centering on steps of survival to decrease mortality and morbidity of this condition.
Recognition and Assessment:
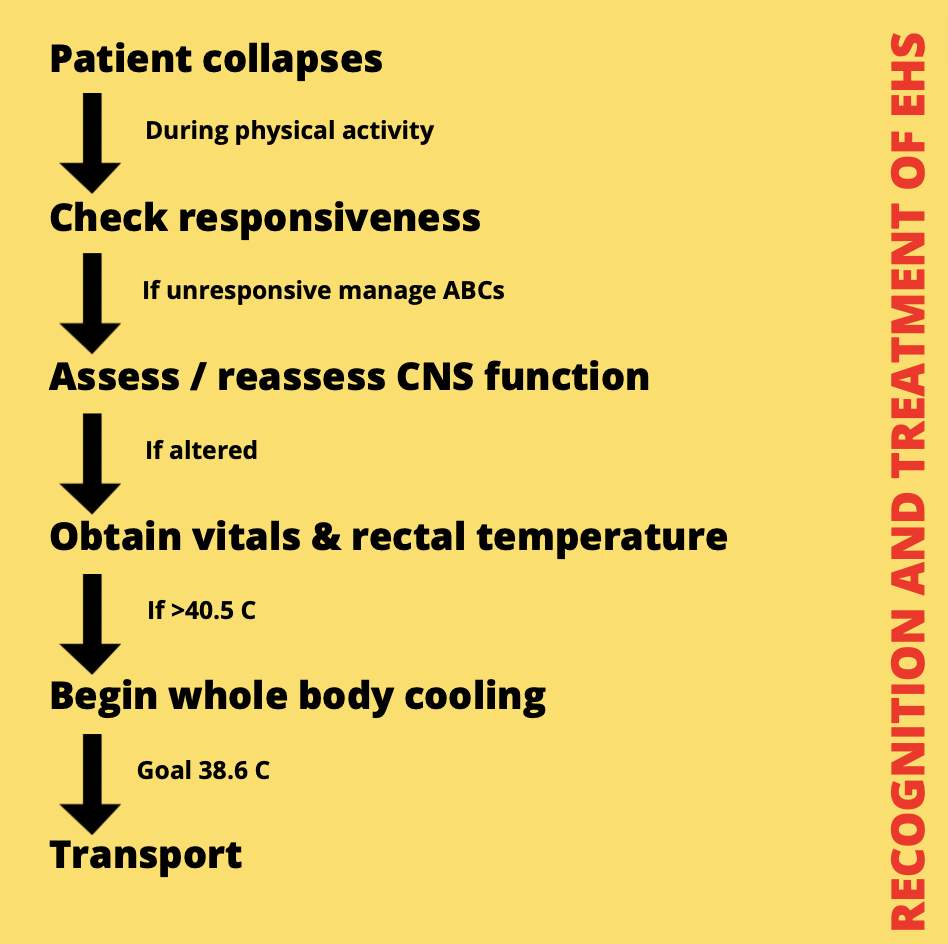
Recognition and treatment of exertional heat stroke. Adapted from Belval et al. 2018
The first step in treating any condition is accurate diagnosis. Early recognition of EHS is key in timely treatment. Laypersons, emergency medical responders, and emergency medical dispatchers all play important roles to identify persons developing EHS. The consensus statement provides a flowsheet to help recognize EHS. Often, the initial recognized symptom is collapse during or after physical activity. After stabilization of all other emergency protocols (such as airway management), CNS function should be assessed. If an abnormal finding like unconsciousness, confusion, combative, irrational behavior, or loss of consciousness is present, a rectal temperature should be obtained with other vital signs. If rectal temperature is greater than 40.5 degrees Celsius with CNS dysfunction, a diagnosis of EHS is made.
Care should be made to consider other causes of CNS depression if the patient’s temperature is not greater than 40.5 degrees Celsius. Additionally, reassessment of the patient’s CNS function should be routinely made as patient’s with EHS often have lucid intervals. Misconceptions about EHS recognition include assertions that a patient with EHS cannot sweat, must have hot skin, and will not be conscious. In reality, patients may be awake, profusely sweating, and feel cool and clammy to the touch.
Physical activity and hot environments can alter temperature readings of patients. Therefore, diagnosis of EHS requires core temperature evaluation. Oral, axillary, aural, tympanic and temporal measurements of temperature is invalid in patients’ at risk for EHS, most often providing lower temperature readings than the actual core temperature. Even though EHS specifies a core temperature reading of 40.5 degrees Celsius or higher, treatment for EHS should not be delayed if a rectal temperature is unable to be obtained, or if the reading is slightly lower than the definitive cut off of 40.5 C.
Treatment:

Cold water immersion should be used to cool a patient with EHS to 38.6 C
The motto of EHS treatment in prehospital settings is “cool first, transport second.” Ideal and goal treatment for EHS is cooling the patient to under 104.5 degrees Fahrenheit in under 30 minutes from time of collapse. This goal is to reduce the end organ dysfunction, morbidity and mortality of this severe hyperthermia. Current best practice to achieve this goal is neck-down cold water immersion, which can be a difficult method in prehospital environments. Dispatchers and first responders should initiate any cooling strategies that are immediately available to anyone suspected of having EHS, until EMS responders can arrive.
The effectiveness of any cooling strategy can be evaluated by its cooling capacity and the body surface area the modality can be applied to. The recommended minimum cooling rate is 0.15 degrees Celsius per minute, yielding 4.5 degrees Celsius in thirty minutes. Cooling should cease when core temperature reaches 38.6 degrees Celsius to decrease the risk of severe hypothermia. Hypothermic overshoot is common; patients should be passively rewarmed to 37 degrees Celsius.
Cold water immersion in ideal conditions can achieve a rate of cooling of 0.35 degrees Celsius per minute, with a practical rate of 0.22 degrees Celsius per minute, as found in a study of 254 EHS cases. Alternative modalities of cooling include tarp-assisted cooling (rate of 0.14-0.17 degrees Celsius per minute), cold shower, fan, and ice packs (which all have < 0.1 degree Celsius per minute cooling rate).
At-risk events, including races and athletic programming, should have advance planning to initiate on-site cooling with adequate staffing. Standard of care for situations with on-site medical personnel (such as physicians or certified athletic trainers) writes for completion of on-site cooling prior to transfer to a hospital for continued medical care.
During transport for patients who are unable to be cooled on-site, the most aggressive and effective cooling method should be undertaken until goal core temperature (rectal 38.6 degrees Celsius) is reached. Cold saline infusion alone is not an adequate cooling strategy and should be implored in conjunction with other cooling techniques.
Additional medical conditions could arise related or unrelated to EHS. Treatment of non-emergent conditions such as emesis should not take priority over initiation and continuation of cooling. Emergent conditions including cardiac arrhythmias and seizures will need to be addressed prior to initiation of cooling with the goal to cool as the priority after stabilization of the patient.
Advanced Care:
Prehospital notification to the receiving facility allows staff to properly prepare for the patient’s treatment upon arrival. Emergency Departments and hospitals will also be able to evaluate for concurrent diagnoses and sequela of EHS. These conditions include rhabdomyolysis, disseminated intravascular coagulation, and liver failure.
How does this affect EMS?
This consensus statement provides an actionable outline of recognition, assessment and treatment of EHS patients. Diagnosis of EHS allows for alteration in EMS typical workflow to optimize the treatment of EHS by cooling. Transportation of patients becomes a secondary goal to treatment.
Bottom Line:
Exertional Heat Stroke is an emergent medical condition that relies on timely treatment in order to reduce morbidity and mortality. EMS is in a unique position to provide rapid recognition, assessment and treatment of these patients.
For additional reading on this topic, please check out: Feel The Heat: Managing Exertional Heat Stroke
Editing by EMS MEd Editor James Li, MD (@JamesLi_17)



