By Kenneth Dumas MD, Johnathon Elkes MD, Rachel Semmons MD
THE CASE
78 year old male with a past medical history of COPD, DMII, HTN, and ESRD currently on hemodialysis calls 911 for complaints of shortness of breath not relieved by his home inhaler. On arrival, the patient is seated on his couch with notable tachypnea at 32 breaths/min. He appears uncomfortable but is alert and speaking full sentences. He denies any chest pain, cough, recent illness, fevers. He is saturating 94% on room air. Blood pressure is 103/74 and HR is 51. Blood glucose is 152. Exam is notable for diffuse wheezing throughout lung fields and a left upper extremity fistula with a palpable thrill. Medications are notable for metoprolol, losartan, Combivent Respimat (ipratropium/albuterol) inhaler, and “some other blood pressure meds”. He last took his metoprolol and the inhaler just prior to arrival without relief of symptoms. The anticipated transport time is 10minutes to the closest facility, which happens to be PCI capable.
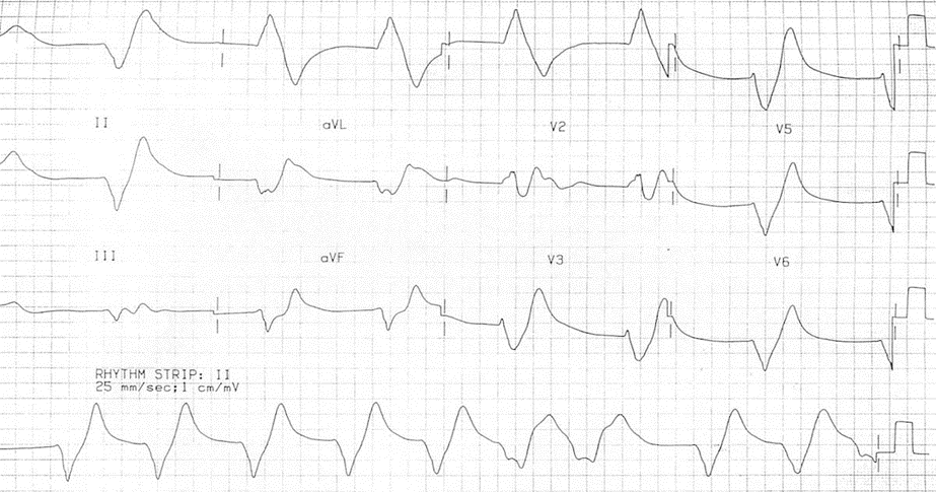
The decision is made to load the patient for transport and begin albuterol/ipratropium nebulizer treatment. While the breathing treatment is being set up an ECG is obtained as below:
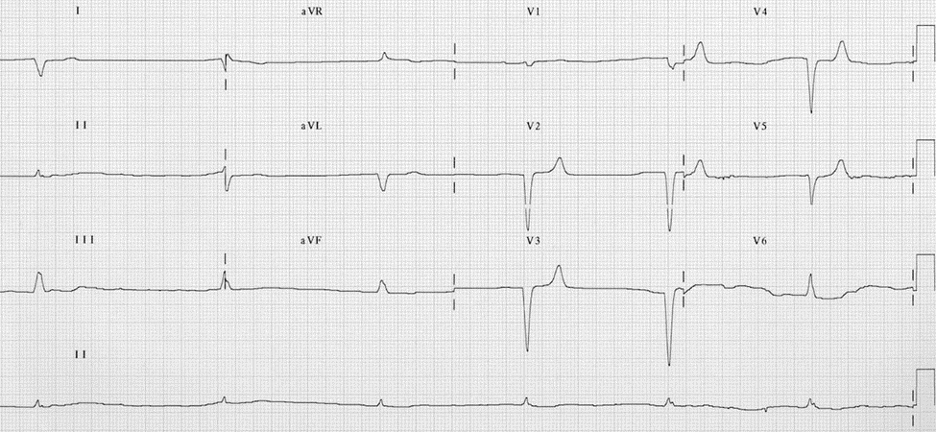
HR 37, QRS duration: 180 ms, PR: n/a, QTc: 346 ms
Currently, the patient is already receiving the nebulized medication. He reports some improvement in shortness of breath and continues to deny any chest pain or other symptoms. He continues to be alert and appropriately interactive. Vitals signs on the monitor are now 48bpm and O2 saturations are now 98%.
What is your differential? What would you do with that ECG?
EVALUATION & LITERATURE REVIEW
It is not uncommon to feel that in our battle against disease, that illness is trying to trick us and stay one step ahead. Before the days of penicillin, syphilis was touted as “the great mimicker”. However, there is a new trickster these days, and a much deadlier one, hyperkalemia. The case above demonstrates just how nonspecific the presentation of hyperkalemia can be. The symptoms are often vague, the patients at risk of hyperkalemia typically have multiple medical comorbidities and the exam is usually benign. Despite the benign history and presentation, this patient presents with a severely deranged EKG. So how do we recognize a potentially life-threatening condition that’s presentation is often varied and non-specific? For this post we reviewed multiple sources to put together key points in the history, physical exam, and EKG interpretation that can help you recognize this deadly condition and place it on your differential early in evaluation. Finally, we discuss emergent treatment options and their mechanisms so that after recognition you can intervene quickly.
HISTORY
Potassium is one of the key electrolytes involved in homeostasis of all cells. Given its widespread involvement it is no surprise that hyperkalemia presents with a wide variety of symptoms. Hyperkalemia can occur through three generalized mechanisms: patients with an increased intake of potassium, patients who are unable to excrete potassium, and those who shift potassium from the intracellular stores to the bloodstream (extracellular shift). Below is a table highlighting some important elements of that patient history that can suggest hyperkalemia through one of these mechanisms.
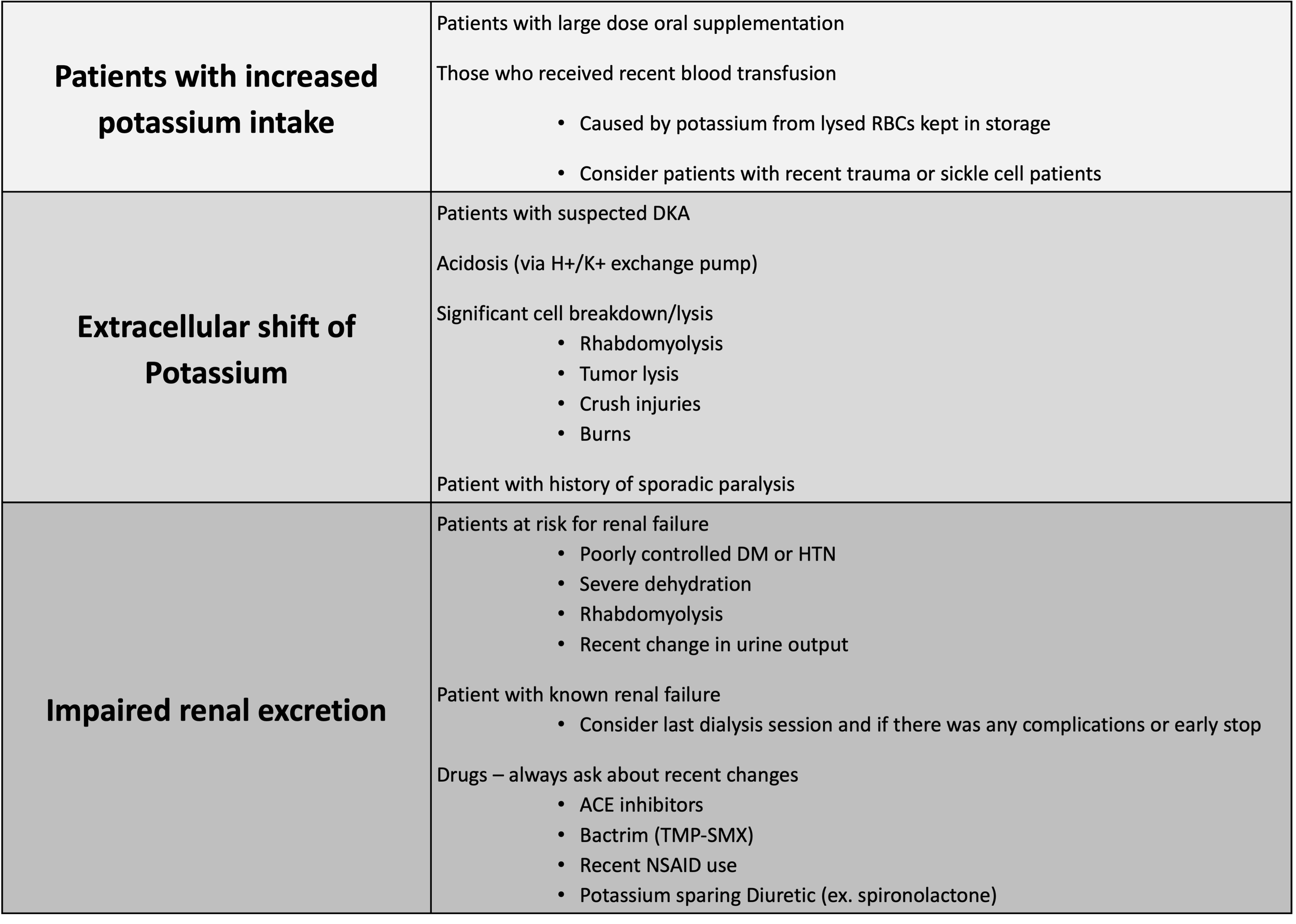
Table 1 [1, 2]
In one study it was noted that 75% of all patients with severe hyperkalemia had renal failure, and 67% were taking a drug that predisposed them to hyperkalemia. [3]
PHYSICAL EXAM
In the prior section, we mentioned features of the history that can help identify hyperkalemia. However, we often do not have the luxury of a complete history from the patient or family in the prehospital setting. Thankfully, there are many physical findings that can increase your suspicion for hyperkalemia
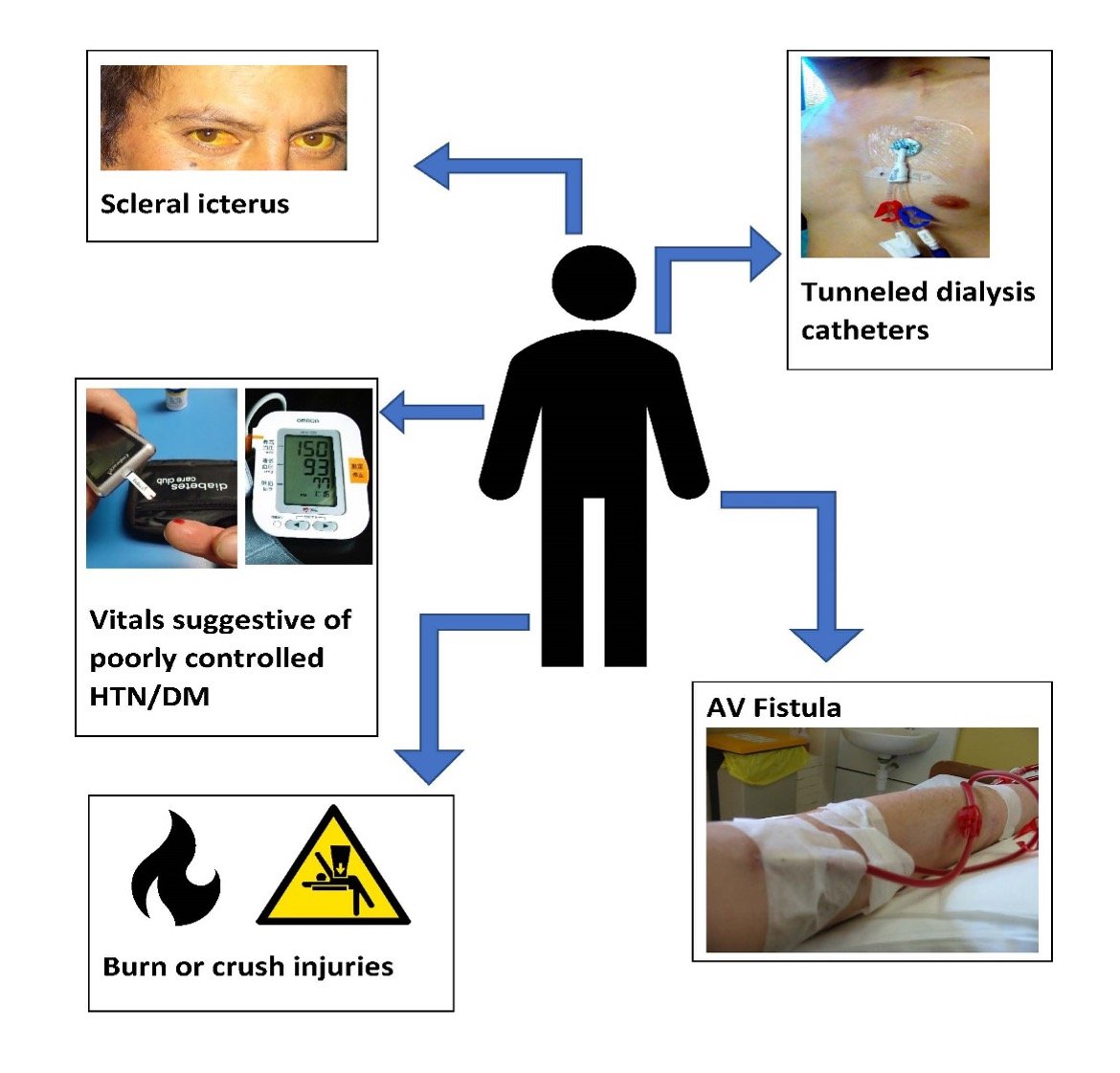
Image 1 [4-9]: Graphic of common exam findings that may be concern for hyperkalemia
-
Indwelling lines: Patients may present with indwelling catheters for various purposes, one of the most common being hemodialysis. If you see a line, consider that this patient may not be excreting potassium as a result of chronic renal failure. Additionally, patients with ports may receive chemotherapy or routine blood transfusions, all of which can place them at higher risk of hyperkalemia.
-
Fistula: Patients with AV fistulas signal that they receive routine hemodialysis, often 2-3 times a week. You can quickly palpate the fistula for a thrill as a quick check to determine if the fistula is working. A patient who missed dialysis or has a dysfunctional fistula is at high risk for hyperkalemia.
-
Burns/Crush injuries: Both can cause significant tissue damage leading to release of intracellular potassium stores into the serum. Furthermore, those with crush injuries may have severe tissue ischemia and breakdown leading to acidosis and release of intracellular potassium. Keep in mind that patients who have had significant downtime or immobilization (i.e. found in the bathtub) may also have significant tissue breakdown.[1]
-
Vitals: Patients who have significantly elevated blood pressures or fingerstick glucose can be a sign of uncontrolled hypertension or diabetes. Both are leading causes of acute renal failure.
-
Scleral icterus: Often an indication of hemolysis, and potential elevated serum levels of potassium. Patients who have scleral icterus may also be routine recipients of blood transfusions and may have increased potassium from the donated products.[2]
-
Cachexia or wasting: Suggestive of malignancy, these patients may have fast growing tumors that outgrow their blood supply and have increased cell turnover with release of intracellular potassium or may be recipients of chemotherapy which can also cause significant cell lysis or even tumor lysis syndrome.[2]
EKG RECOGNITION:
Finally, one of the most powerful tools available in the field for recognition of hyperkalemia is the EKG. Unlike some other diseases, there is not one single pathognomonic EKG finding but rather a spectrum of changes.
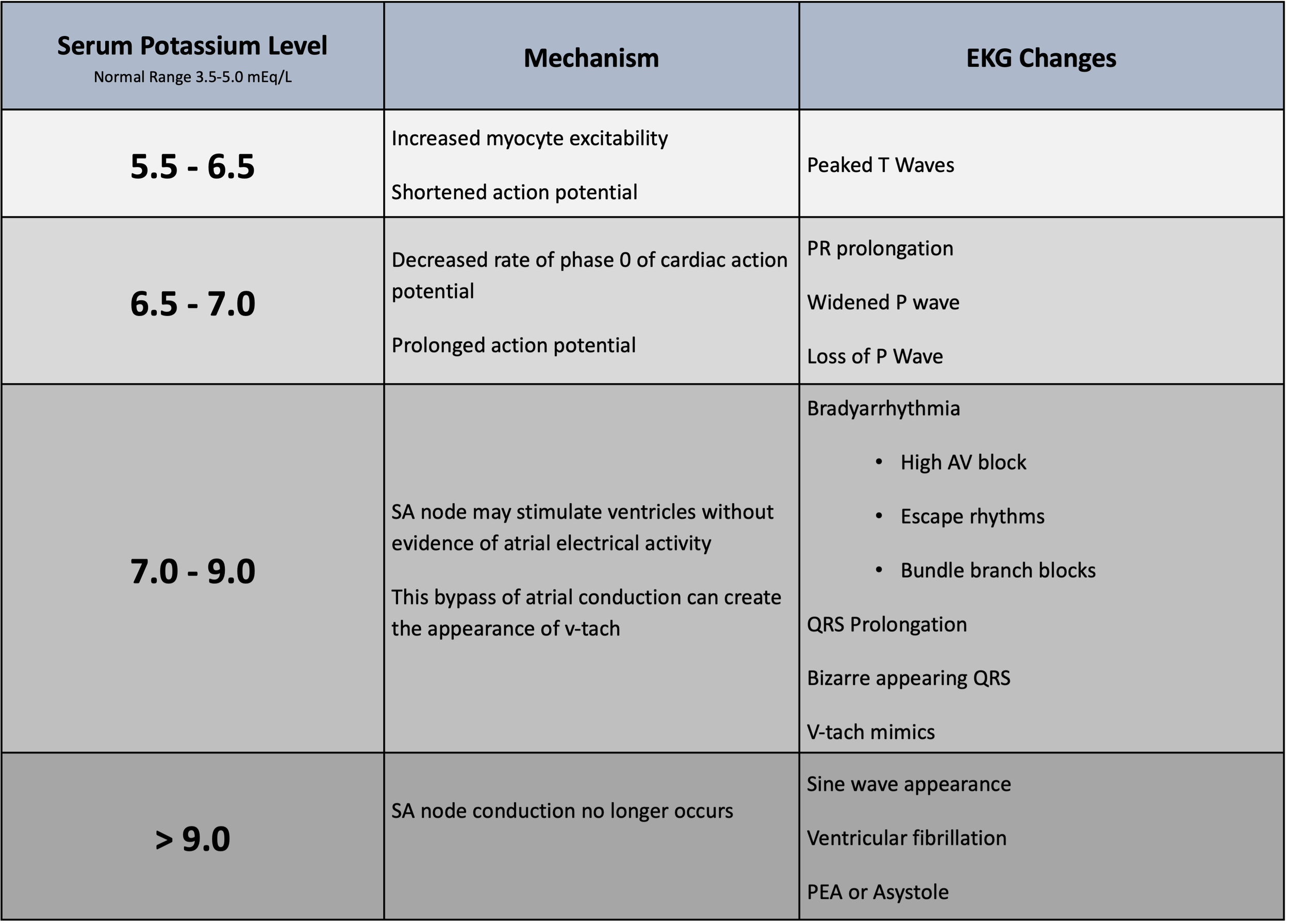
Table 2 [2, 10]
So, let’s look at some real-world examples of these changes that you might one day encounter in the patient with hyperkalemia.
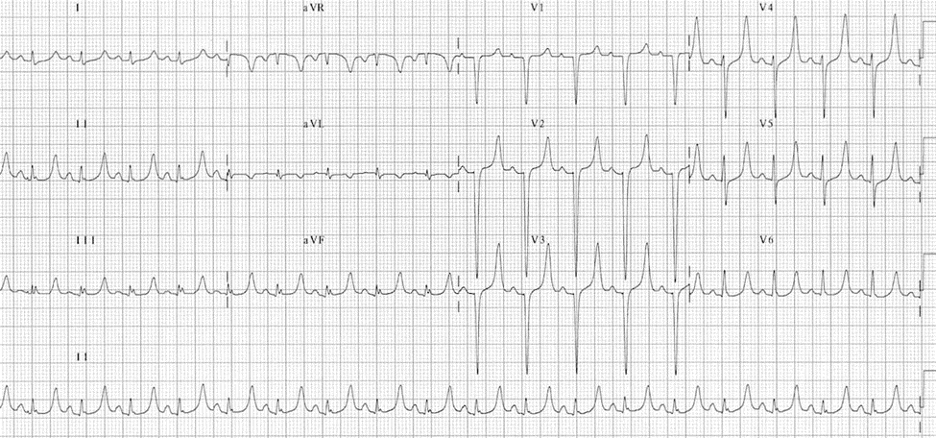
EKG 1 – Demonstrates peaked T-waves in a patient with hyperkalemia. Usually best seen in leads II, III, and V2-V4. Note these may only present in 22% of patients with hyperkalemia [10] EKG from LITFL [11]
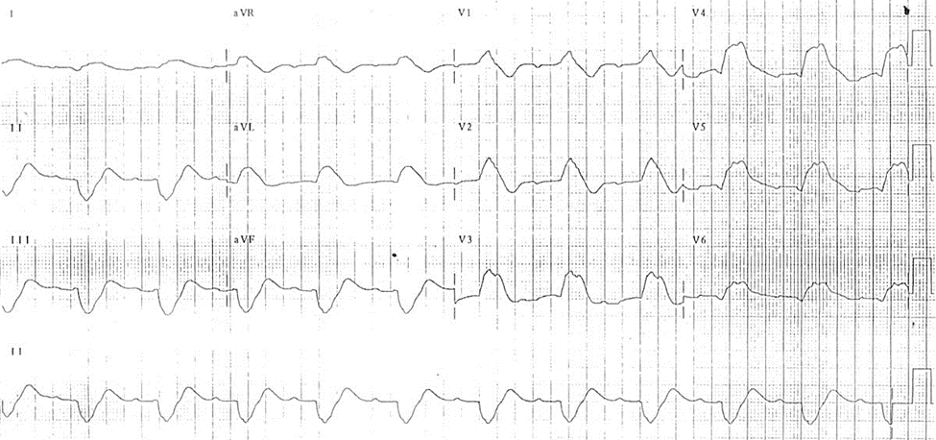
ECG 2- This EKG shows some of the bizarre QRS complexes that can form as hyperkalemia worsens. You can distinguish this morphology from right and left bundle branch blocks because the QRS will be uniformly wide, rather than just the initial or terminal portion. [10] EKG from LITFL [11]
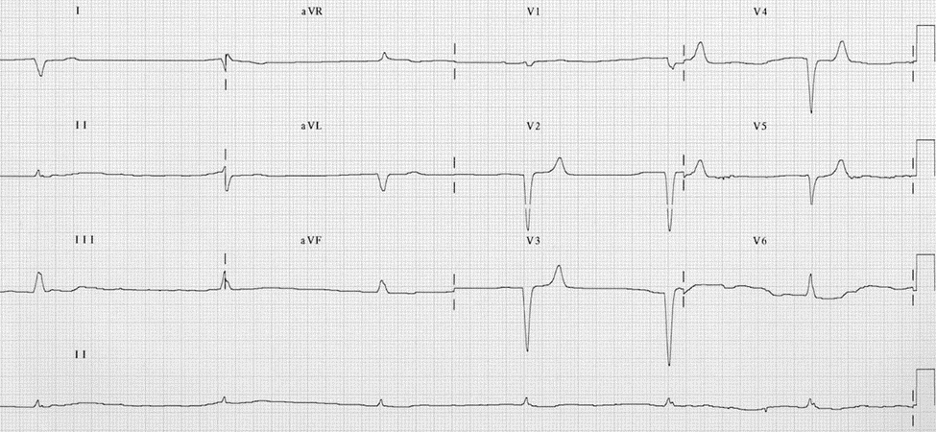
EKG 3 – Note the extreme bradycardia in this EKG along with absence of P waves. This EKG shows the effect of severe hyperkalemia, where SA conduction no longer occurs, and electrical stimulation is left to the junctional pacemakers [10] EKG from LITFL [11]
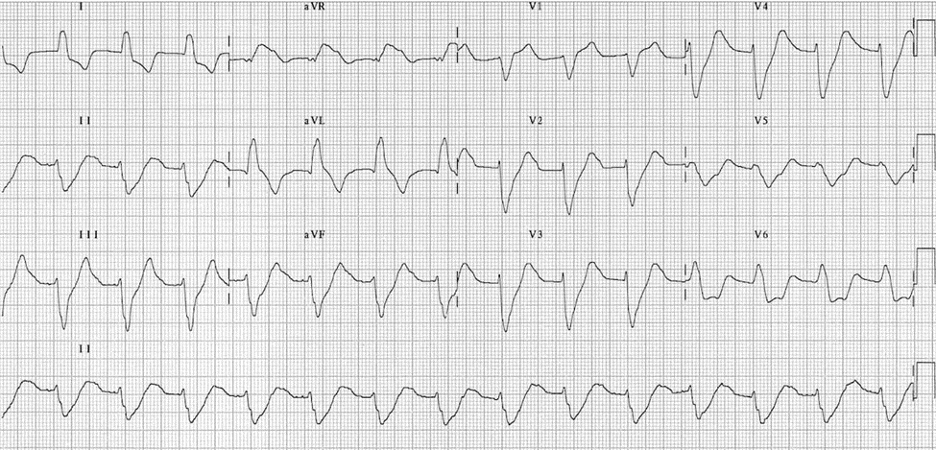
EKG 4 – This EKG is a great example of a V-tach mimic. This can occur as electrical stimulation from the SA node bypasses the atria and stimulates the ventricles, noted by a wide regular rhythm with absence of p-waves.[10] While V-tach should be considered in patients with a regular wide complex rhythm, this EKG is only showing a rate of 84 BPM, making it extremely suggestive of hyperkalemia in the right patient presentation.
EKG from LITFL [11]
EKG 5- Finally, this is a rhythm you hope to never see, because it is an omen that asystole or PEA is just around the corner. This is the “sine-wave” pattern that is associated with extreme hyperkalemia. The sine pattern is caused by the blending of QRS complexes and T-waves.
EKG from LITFL [11]
TREATMENT
So now that you have an idea of how to recognize hyperkalemia in the field, more importantly, what can you do about it? Ultimately some of these patients may require hemodialysis (HD) but that requires transport to a facility with dialysis capability. There are a few critical interventions you can perform to help stabilize and ultimately buy these patients time. Keep in mind these treatments have short durations and may need to be re-dosed for long or delayed transports.
Calcium: Perhaps the most critical is the administration of calcium. Calcium’s effect is almost immediate and works to stabilize the cardiac membrane and prevent severe arrhythmias. [2] There is some concern giving calcium chloride through a peripheral line as extravasation can cause tissue damage and necrosis so it should be given through a well-established peripheral line. However, the benefit of calcium in the case of hyperkalemia outweighs the risk of possible extravasation
Albuterol: Once the membrane is stabilized the next goal is to shift serum potassium back into the intracellular space. Albuterol works as its Beta-2 agonist properties stimulate the Na-K ATPase pump promoting the intracellular transport of K. [2] This requires a significant amount of albuterol, approximately 10-20mg, so a normal COPD/Asthma dose will not be sufficient in these cases. [1] Albuterol has the benefit of being inhaled so even in patients whom access is unable to be obtained, you can provide treatment.
Insulin: Insulin works in a way similar to albuterol, stimulating the Na-K ATPase to promote intracellular shift of potassium. [2]This is given as an IV dose. Current literature suggests starting with 5 units of insulin and co-administration of 2 amps (50G) of dextrose to prevent hypoglycemia. [12] If a patient is already hyperglycemic dextrose need not be administered but routine fingerstick glucose monitoring should be performed to prevent severe hypoglycemia.
Insulin is not routinely available to most pre-hospital providers however, it is important to recognize the mechanism, duration of action, and risk of hypoglycemia associated with its use. Patients who are being transferred interfacility may have received these therapies and transport time may be longer than the duration of action and re-administration should be considered.
Sodium Bicarbonate: This is perhaps the most debated topic when it comes to treatment for hyperkalemia. It is theorized that bicarb promotes intracellular shift of potassium via the H/K transporter and via Na/HCO3- cotransporter. [12]. There is some debate surrounding the use of sodium bicarbonate with regards to the exact mechanism, how effective it is, and how it should be given. That said, when treating hyperkalemia if you have: a critical patient, a patient who you suspect may be acidotic, or patient refractory to other measures, sodium bicarbonate can potentially provide benefit and should still be given.
Medications to avoid: Guidelines are great, they help us guide care in especially stressful situations. In the case of hyperkalemia there are medications used in critically ill patients that are often considered standard of care (i.e. ACLS) that should be avoided. Succinylcholine can acutely precipitate hyperkalemia and sodium channel blocking agents (procainamide, lidocaine, and amiodarone) can be deadly in the setting of hyperkalemia [13]
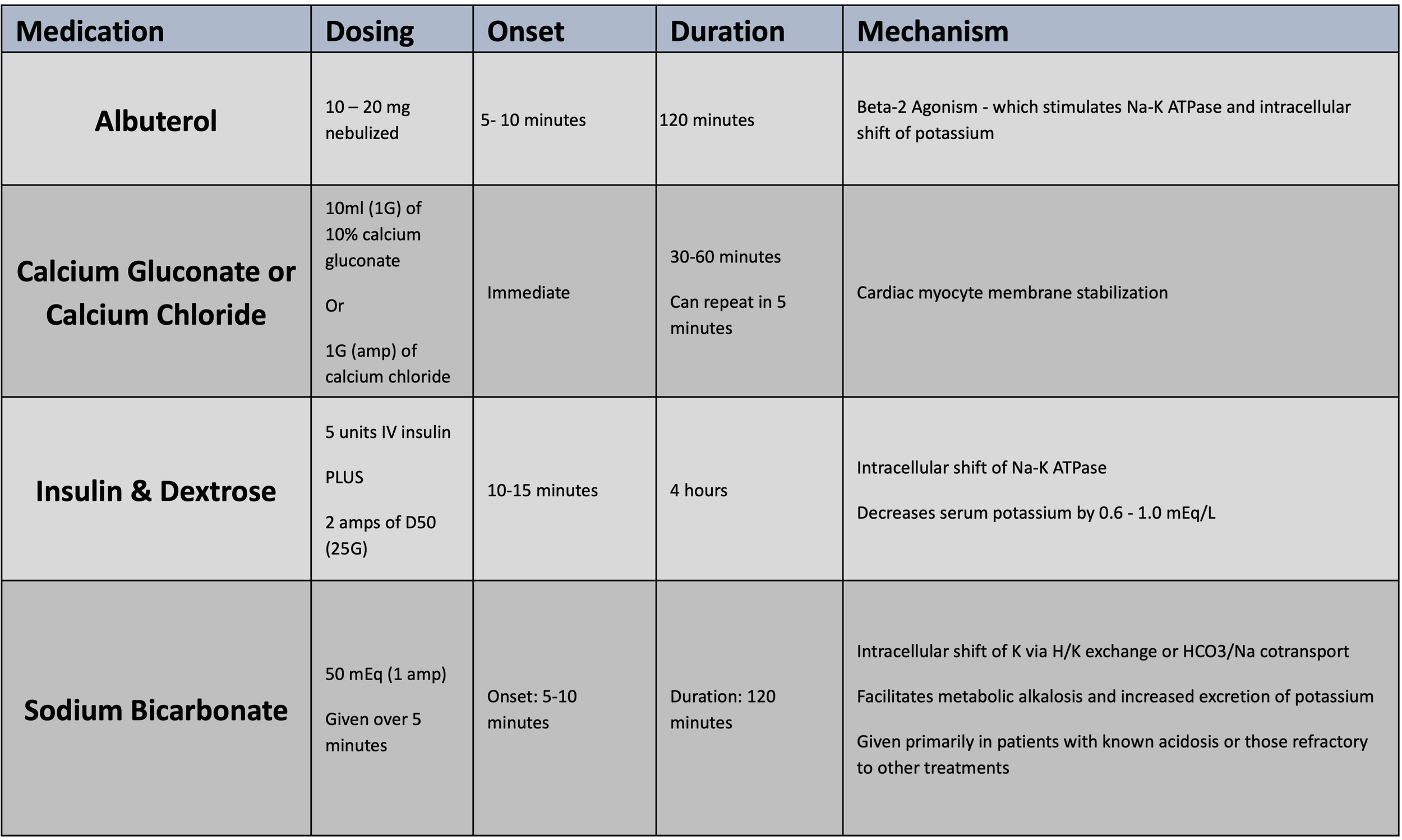
Table 3 [1, 2, 10]
CASE CONCLUSIONS:
The patient arrived at the ER 10 minutes later. Physical exam was significant for HR 35, diaphoresis, tachypnea, and BP 107/78. His mental status remains very alert and interactive, but he is in mild distress. He receives 2g calcium chloride immediately. A point-of-care blood gas displays a potassium level of NA. Discussion with the patient reveals his last HD episode was 5 days ago but was stopped early due to patient request. Nephrology is paged to begin preparations for emergent dialysis. The patient is given insulin, D50, and sodium bicarbonate, which stabilized him. Finally the patient was able to be taken to hemodialysis for further care and resolution of electrolyte abnormality.
For more on the related topic of approach to bradycardia (& hyperkalemia) see this article from the Cognitive Awareness case series.
REFERENCES
1. Harwood-Nuss\’ Clinical Practice of Emergency Medicine. 6th Edition 2015.
2. Petrino R, Marino R. Fluids and Electrolytes. In: Tintinalli JE, Ma OJ, Yealy DM, et al., eds. Tintinalli\’s Emergency Medicine: A Comprehensive Study Guide, 9e. New York, NY: McGraw-Hill Education, 2020.
3. Acker CG, Johnson JP, Palevsky PM, Greenberg A. Hyperkalemia in Hospitalized Patients: Causes, Adequacy of Treatment, and Results of an Attempt to Improve Physician Compliance With Published Therapy Guidelines. Archives of Internal Medicine 1998;158(8):917-24 doi: 10.1001/archinte.158.8.917.
4. contributors WC. Sodium Bicarbonate. In: (1).JPG FSB, ed. Wikimedia Commons: Wikimedia Commons, the free media repository.
5. contributors WC. Scleral icterus. In: Icterus.jpg FS, ed.: Wikimedia Commons, the free media repository.
6. contributors WC. Plugged into dialysis. In: dialysis.jpg FPi, ed.: Wikimedia Commons, the free media repository.
7. contributors WC. Hickman line catheter with 2 lumens. In: lumens.jpg FHlcw, ed.: Wikimedia Commons, the free media repository.
8. contributors WC. Omron HEM-7000. In: 20110121.jpg FOH-, ed.: Wikimedia Commons, the free media repository.
9. contributors WC. Device to check for diabetes. In: 2.jpg FDtcfd, ed.: Wikimedia Commons, the free media repository.
10. Parham WA, Mehdirad AA, Biermann KM, Fredman CS. Hyperkalemia revisited. Tex Heart Inst J 2006;33(1):40-47.
11. Robert Buttner EB. hyperkalemia. Secondary hyperkalemia [Website] Mar 24 2022. https://litfl.com/hyperkalaemia-ecg-library/.
12. Farkas J. Management of severe hyperkalemia in the post-Kayexalate era. EMCrit: Metasin LLC, 2015.
13. Reka Zsilinska KS. Ventricular Tachycardia Mimics. In: Alex Koyfman BL, ed. emDocs, 2017.
Editing by EMS MEd Editor James Li MD (@JamesLi_17)



