What’s the Big Picture?
By Adrien Quant LP, Hashim Q. Zaidi MD
As discussed in Part 1 and Part 2, current EMT standards of lung auscultation and pulse oximetry have critical limitations in the evaluation of ventilation and perfusion (Brown et al., 1997; DeMeulenaere 2007; Chan et al., 2013). However, the introduction of waveform capnography to the EMT scope of practice would largely resolve these issues. The introduction of waveform capnography is necessary to promote the evidence-based nature of EMS healthcare, and improve prehospital care in regions of the United States where EMTs are the highest level providers.
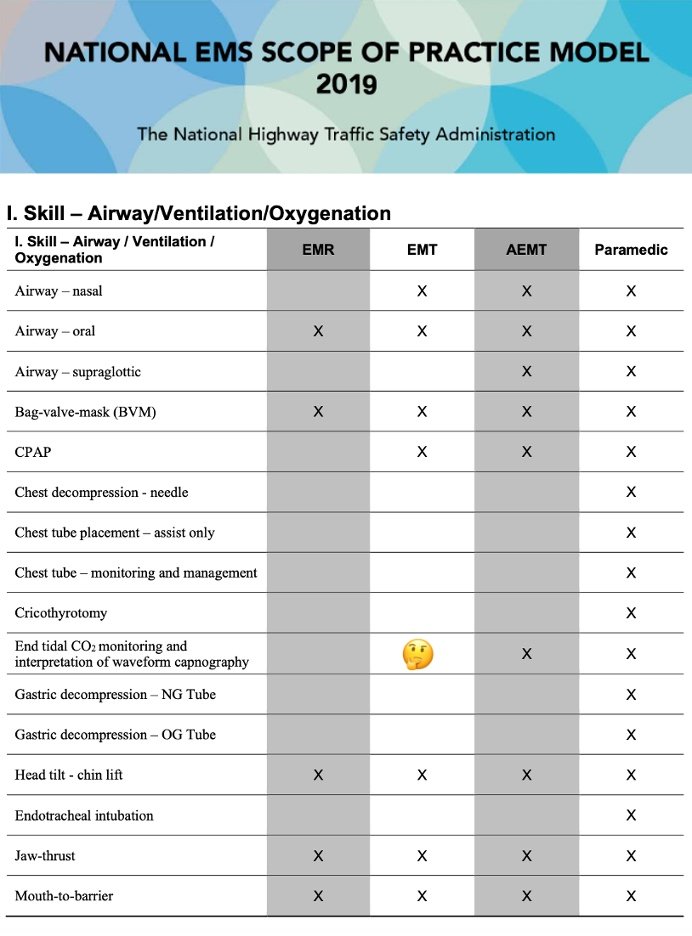
Skill – Airway/Ventilation/Oxygenation (Modified)
Source: National EMS Scope of Practice Model 2019
https://www.ems.gov/pdf/National_EMS_Scope_of_Practice_Model_2019.pdf
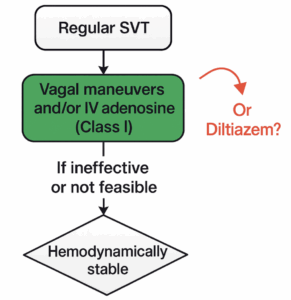
In the emergency department, waveform capnography is the gold standard to determine whether an airway intervention has been effective. In fact, the technology is repeatedly endorsed by the new NAEMSP Airway Compendium, particularly for non-invasive positive pressure ventilations (Carlson et al., 2022; Harris et al., 2022; Lyng et al. 2022). When the National EMS Scope of Practice Model (2019) was constructed, the Expert Panel placed waveform capnography in the ALS scope of practice. Why was it left out of the EMT scope of practice?
Incidentally, the Expert Panel did consider placing waveform capnography into the EMT scope of practice (National, 2019). During the development of the guidelines, the Expert Panel considered placing supraglottic airways into the EMT scope of practice. Since supraglottic airway placement requires waveform capnography confirmation, the panel also considered including waveform capnography into the EMT scope of practice as well. However, the panel ultimately decided against supraglottic airway implementation, citing concerns that supraglottic airways can harm patient outcomes if improperly placed by an EMT. In addition, the cost of supraglottic airways could be cost prohibitive to many EMT educational programs. As such, the panel decided against including supraglottic airways into the EMT scope of practice due to clinical and financial concerns. Unfortunately, when the panel decided to exclude supraglottic airways, the panel also decided to exclude waveform capnography. This was a curious decision. Whether supraglottic airways are dangerous or cost prohibitive for EMTs is a valid concern for separate discussion; however, the extensive benefits of waveform capnography justifies its cost. The exclusion of supraglottic airways from the EMT scope of practice should not have facilitated the exclusion of waveform capnography. These are separate technologies with different costs and risk/benefit ratios. Arguably every EMT level airway intervention (manual airway maneuvers, bronchodilator and epinephrine administration, supplemental oxygen administration, CPAP administration, and positive pressure ventilations) could benefit from waveform capnography validation.
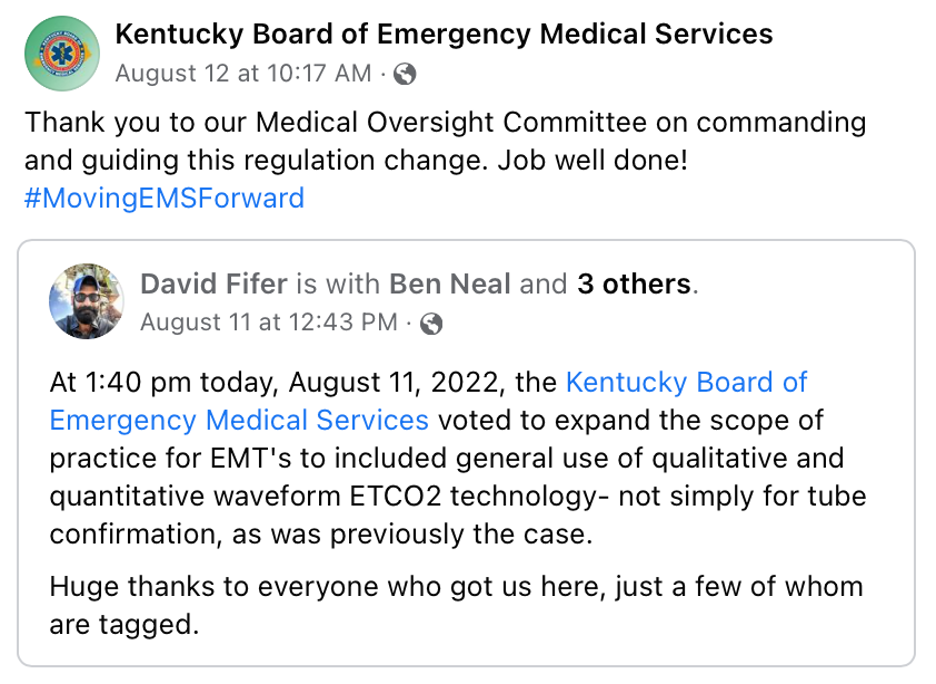
Under new regulation KBEMS-E-39, Kentucky now mandates supplemental training of non-invasive qualitative and quantitative waveform capnography for EMTs.
Source: Kentucky Board of Emergency Medical Services & David Fifer
https://www.facebook.com/KYBoardEMS
Fortunately, improvements are on the way. On August 11, 2022, the Kentucky Board of Emergency Medical Services expanded waveform capnography to the EMT level (Kentucky 2022). Under new regulation KBEMS-E-39, Kentucky now mandates supplemental training of non-invasive qualitative and quantitative waveform capnography for EMTs. Under this new order, EMTs will be trained to utilize waveform capnography to evaluate the quality of their BLS interventions. In our opinion, this is a critical first step towards improving patient care across the state. The United States should follow Kentucky’s evidence-based change.
In closing, waveform capnography should be included into the national EMT scope of practice. As stated by the National EMS Scope of Practice Model (2019), “depending on a patient’s needs and/or system resources, EMTs are sometimes the highest level of care a patient will receive during an ambulance transport.” As such, many patients, especially in rural parts of the United States, are being treated by EMTs who are ill equipped to appropriately evaluate their airway and breathing interventions. Lung auscultation and pulse oximetry are simply not enough. In order to empower our EMT providers and elevate our patient care, we must include waveform capnography in the EMT scope of practice.
Check out Part 1 and Part 2
References:
1. Brown LH, Gough JE, Bryan-Berg DM, Hunt RC. (1997). Assessment of Breath Sounds During Ambulance Transport. Annals of Emergency Medicine, 29(2), 228–231. https://doi.org/10.1016/S0196-0644(97)70273-7
2. Chan E, Chan M, Chan M. (2013). Pulse oximetry: Understanding its Basic Principles Facilitates Appreciation of its Limitations. Respiratory Medicine, 107(6), 789–799. https://doi.org/10.1016/j.rmed.2013.02.004
3. DeMeulenaere S. (2007). Pulse Oximetry: Uses and Limitations. The Journal for Nurse Practitioners, 3(5), 312–317. https://doi.org/10.1016/j.nurpra.2007.02.021
4. Carlson J, Colella M, Daya M, De Maio V, Nawrocki P, Nikolla D, Bosson N. (2022). Prehospital Cardiac Arrest Airway Management: An NAEMSP Position Statement and Resource Document. Prehospital Emergency Care, 26(sup1), 54–63. DOI: 10.1080/10903127.2021.1971349
5. Harris M, Lyng JW, Mandt M, Moore B, Gross T, Gausche-Hill M, & Donofrio-Odmann JJ. (2022). Prehospital Pediatric Respiratory Distress and Airway Management Interventions: An NAEMSP Position Statement and Resource Document. Prehospital Emergency Care, 26(sup1), 118–128. https://doi.org/10.1080/10903127.2021.1994675
6. Kentucky Board of Emergency Medical Services (2022). Statement of Emergency, 202 KAR 7:701E. https://apps.legislature.ky.gov/law/kar/titles/202/007/701/
7. Kentucky Board of Emergency Medical Services (2022). Thank you to our Medical Oversight Committee on commanding and guiding this regulation change. Facebook. https://www.facebook.com/KYBoardEMS
8. Lyng J, Harris M, Mandt M, Moore B, Gross T, Gausche-Hill M, Donofrio-Odmann JJ. (2022). Prehospital Pediatric Respiratory Distress and Airway Management Training and Education: An NAEMSP Position Statement and Resource Document. Prehospital Emergency Care, 26(sup1), 102–110. https://doi.org/10.1080/10903127.2021.1992551
9. National Highway Traffic Safety Administration. (2019). National EMS Scope of Practice Model. https://www.ems.gov/pdf/National_EMS_Scope_of_Practice_Model_2019.pdf
Editing by EMS MEd Editor James Li, MD (@JamesLi_17)