By Tiffany Pleasent, MD
Case Review
A 64-year-old female calls 911 for severe shortness of breath and chest pain. An ALS crew arrives on scene to find a woman who is tachypneic, hypoxic, tachycardic, and hypotensive, with diffuse rales and rhonchi throughout her lung fields. She becomes altered and severely hypoxic. The attending paramedics begin bag-valve-mask (BVM) ventilation, correct her hypoxia and hypotension, and subsequently intubate her on scene with ketamine and rocuronium. This is followed by appropriate confirmation with waveform capnography and all other appropriate adjuncts. Upon arrival to the ambulance, the EMT notices that the patient’s heart rate is 22 bpm. Shortly after they discover that she is pulseless and apneic. They begin CPR en route to the emergency department where the patient’s rhythm deteriorates into asystole. Further resuscitation is futile, and she dies.
The ER physician in the destination emergency room determines that the endotracheal tube was misplaced in the esophagus. This EMS system promotes a “just culture” that influences the crew to self-report their difficult cases to medical direction for evaluation and feedback.
The EMS medical director reviews the case and its associated monitor file which includes the timing and quality of all vital signs, including chest compression depth and rate. The monitor file shows an initial 4-phase waveform capnography of 25 mmHg for 8 breaths immediately following intubation. It further shows a subsequent loss of end-tidal waveform. This is followed by an abrupt bradycardia occurring simultaneously with rapidly dropping SpO2. The period between loss of initial waveform capnography and initiation of chest compressions was over 7 minutes. The endotracheal tube was never evaluated, removed, nor exchanged in the field.
The EMS medical director wonders if this is a “one-off” case or an indicator of more systemic issues. She decides to evaluate other similar cases and discovers that 5% of all intubations in her system lose waveform capnography and progress to cardiac arrest. She decides to implement system-level changes to manage these cases.
Keeping patient safety as our priority
Application of a systematic approach to quality improvement allows us to do the greatest good for the greatest number of people on a consistent basis. The case above describes a system with multiple unrecognized failed airways (UFAs), some likely resulting in patient harm. Fortunately, the medical director and the service leadership have a committed desire to implement change.
Several considerations arise:
-
How does the medical director develop ideas and choose what she wants to change in order to decrease UFAs?
-
How should she know what to monitor?
-
Should she use qualitative or quantitative data to drive system change?
-
How frequently should she be analyzing the data?
-
How does she appropriately analyze the data in order to obtain the right information? When should she abort a change idea?
-
How does she know that an improvement truly is an improvement?
Both EMS physician and EMS clinician involvement are required in this process, and the system is best served when both understand key quality management principles.
What are some key quality management principles that are applicable to EMS?
The Model for Improvement
The Institute of Medicine’s (now known as the National Academy of Medicine) Model for Improvement was initially adopted from the Associates in Process Improvement as a commonly used framework for healthcare providers to improve their systems [5,7,8]. It requires clinicians a) to create a measurable aim, b) to establish quantifiable measures that can be used to evaluate improvement over time, and c) to develop change ideas to implement. This is followed by small-scale tests of change using PDSA (plan-do-study-act) cycles that are scalable if the cycle is successful.
The difference between quality improvement and quality assurance
These two terms are frequently used interchangeably, albeit incorrectly. Quality assurance describes the detection of an error after the error has occurred [8]. Quality improvement describes evaluation of the system to ensure it appropriately produces the desired results and prioritizes error avoidance. Quality improvement is proactive whereas quality assurance is reactive, and both are important.
Case Review Application
The medical director decides to apply small tests of change to improve her system. She creates an aim statement, establishes quantifiable outcome measures, and develops several change ideas. Following implementation of each change idea, she says “show me the data!”
PDSA Cycles
#1 – An e-mail memo is sent to the EMS system reminding clinicians to establish and monitor continuous waveform capnography of all airway devices while en-route to the hospital and during patient movement and handoffs. After one month, there is no change in the system’s UFA outcome measures.
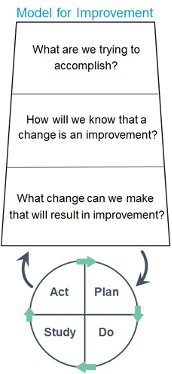
Model for Improvement: PDSA Cycle (Institute for Healthcare Improvement)
#2 – A podcast is developed explaining waveform capnography and the importance of continuous monitoring of advanced airways. Additionally, a protocol revision is made outlining advanced airway confirmation and management requirements. Unfortunately, there is minimal change in the UFA outcome measures.
#3 – To identify further change theories, the medical director facilitates a case review with the EMS clinicians involved in each of the UFA cases that resulted in cardiac arrest. Nearly all the crews recall difficulty seeing the cardiac monitor in their ambulances due to the monitor mount being poorly positioned. Furthermore, they report their monitor never alarmed that capnography was lost. Clinicians provide recommendations for better placement of the mount in the ambulance and the change is made to the entire fleet. Crews report in the following weeks a significant improvement in their ability to monitor their patient.
#4 – The cardiac monitor settings are reviewed and nearly all alarms have been turned off by crews because of frequent inappropriate alarms resulting in alarm fatigue. The team involves EMS clinicians to identify the most important alarms to maintain, including the capnography apnea alarm, and an admin password is established to prevent these settings from being changed. These monitor changes are trialed by a group of crews for a few shifts and additional small refinements are made based on their feedback prior to deployment on all the system’s monitors.
There is subsequently a dramatic and sustained system-wide improvement and no further UFAs occur over the next year.
The EMS physician and the EMS clinician are key players in quality improvement
While this case example presents an example of a single quality improvement project, there are innumerable opportunities for improvement among the diversity of EMS systems worldwide. The process of improving healthcare delivery is most efficient when there is valuable input and advocacy from both EMS physicians and EMS clinicians. Understanding of quality management fundamentals begins with initial education.
In the above case, imagine if the EMS clinicians’ initial education taught the importance of and the process by which system improvement is achieved. Several considerations arise:
-
Would they have been proactive in telling her their difficulty in seeing the monitor?
-
Would someone have told her how the unnecessary alarms caused them to turn all alarms off on all of their monitors?
-
Would there be increased compliance and accuracy of documentation within electronic health records that are used for quality improvement & research?
-
Could this swing the pendulum from seeking buy-in to achieving advocacy among key stakeholders?
The most efficient shift from quality assurance to quality improvement requires input from the “boots on the ground” who offer critical perspective and input regarding their needs and challenges in delivering healthcare within the vision and oversight of the EMS physician. If the fundamentals of quality management were provided in initial education, the impact would be profound.
Should we integrate quality improvement concepts within EMS education?
Yes! The Future of EMS begins NOW!
As new EMS medical directors and EMS clinicians enter the workforce, it is incumbent upon their educators – including educators for the medical directors – to provide the skills that are required to be successful in this changing healthcare environment. Educators should be trained in key quality improvement concepts, which include tools that may be infrequently taught in traditional healthcare-related settings. Examples include process control charts and other data analysis skills. We must maintain a systematic, data-driven, and evidence-based approach to system quality management and performance improvement [1,2,3,5]. Within our evolving healthcare climate, this effort requires creativity and innovation.
The EMS Agenda 2050 describes six guiding principles to its “people-centered vision for the future of emergency medical services.” These include: inherently safe and effective, integrated and seamless, reliable and prepared, socially equitable, sustainable and efficient, and adaptable and innovative [3]. As outlined in the NAEMSP position statement “Defining Quality in EMS”, we must provide quality and value-based assessments of care in an evidence-based manner which prioritizes patient outcomes [2]. We must be uniform in our terminology and presentation of data, and we must utilize evidence-based methods through open and transparent communication. In order to meet these goals, we must ensure these core principles are provided within our foundation – our EMS education.
Edited by: Jeffrey Jarvis, MD, EMT-P; Ray Fowler, MD, FACEP, FAEMS; Brian Miller, MD; and Al Lulla, MD
References:
1. Crowe RP, Jarvis JL. Quality Improvement and Research. Prehospital Emergency Medicine Secrets. Elsevier; 2022:18-21.
2. Defining Quality in EMS. Prehosp Emerg Care. 2018; 22: 782-783.
3. EMS Agenda 2050 Technical Expert Panel. EMS Agenda 2050: A People-Centered Vision for the Future of Emergency Medical Services. Washington, DC: National Highway Traffic Safety Administration, 2019.
4. Institute for Healthcare Improvement. Science of Improvement: How to Improve. 2023. Available at: https://www.ihi.org/resources/Pages/HowtoImprove/ScienceofImprovement
HowtoImprove.aspx. Accessed January 30, 2023.
5. Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academies Press, 2001.
6. Lincoln EW, Reed-Schrader E, Jarvis JL. EMS, Quality Improvement Programs. Stat Pearls. Published online January 2022. https://www.statpearls.com/point-of-care/31814
7. Langley GJ, Nolan TW, Provost LP, Nolan KM, Norman CL. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco, CA: Wiley 1996.
8. Crowe RP. The evolution of quality concepts and methods. Emergency Medical Services: Clinical Practice and Systems Oversight. 2021; 112: 424-431.
Website Editing and Layout by EMS MEd Editor James Li, MD



