By A.J. Meyer MD
Clinical Scenario
You are dispatched to a 57-year-old male with a witnessed cardiac arrest and bystander CPR being performed. On arrival to the scene, you find the patient pulseless and apneic. Your Fire Department colleagues take control of the airway and begin ventilating the patient with a BVM and perform high quality chest compressions. Your partner deploys the cardiac monitor and while CPR is continued you turn your attention to establishing vascular access. In the midst of the cardiac arrest, you have difficulty obtaining IV access. Subsequently, IO access is successfully established.
Background
Despite conflicting literature to support some pharmacological therapies in out of hospital cardiac arrest, the American Heart Association (AHA) currently recommends obtaining vascular access intravenously or intraosseously in cardiac arrest. [1] The Adult Cardiac Arrest ACLS algorithm currently includes epinephrine and either amiodarone or lidocaine as recommended pharmacologic therapies. Given that the AHA guidelines serve as the standard of care for cardiac arrest management in the United States, this highlights the importance establishing vascular access for administration of pharmacologic therapy in cardiac arrest. The AHA further specifies that IV access is the preferred route; however, IO access is acceptable if unable to obtain IV access. [2] The case of being unable to establish IV access and having to “settle” for IO access brings up an important question: Does your site of access matter in cardiac arrest? Or in other words, is IO access inferior to IV access? Below, we will examine the current literature.
IV vs IO Access Time and Success Rate
There are a number of patient populations in which IV access may be difficult to obtain. Patients in cardiac arrest certainly are no exception. Patient factors including vascular collapse and environmental factors such as tight spaces and moving ambulances contribute to the challenge of obtaining intravenous access in the prehospital setting. [3] In 2007, the NAEMSP released a position statement recognizing these challenges, and subsequently reemphasized the use of intraosseous vascular access in the prehospital setting when there is difficult or delayed vascular access, such as in cardiac arrest patients. Delayed vascular access may limit the benefit of pharmacologic therapies due to late administration. One study showed that average time to establish an IV in the prehospital setting was 4.4 minutes. [4] Times can be expected to be further delayed in cardiac arrest. A retrospective data review of the out-of-hospital cardiac arrest (OHCA) database from 2013-2015 demonstrated statistically significant differences in time from patient contact to administration of epinephrine between IV and IO groups (8.8 minutes versus 5.4 minutes). [5] Further, first attempt success rate of tibial IO access in cardiac arrest patients was significantly higher at 91% compared to 43% for IV access in another study. [6]
Thus far, IO access seems to have a competitive edge over IV, but does the specific site of IO access matter? Reades et. al answered this question with a prospective observational study which showed a significantly shorter time interval to obtain tibial IO access (4.6 minutes) compared to humeral IO access (7.0 minutes). Amount of fluid infused was similar for tibial and humeral sites, but first-attempt success rates for humeral access were only 50%, and humeral IO dislodgment occurred 20% of the time, likely secondary to being in close proximity to the upper torso where the majority of the resuscitation efforts take place. [6] In terms of flow rates, large bore IV access certainly is superior, while the flow rates of IO access has been estimated to be similar to that of a 21-gauge IV catheter. [4] Of note, there have been studies with swine models that showed significantly higher flow rates at the humeral site.
Pharmacokinetics
Despite differing flow rates between IO and IV sites, studies have shown similar effects and serum drug levels between the two. [4] Cameron et. al confirmed that injection of a radionuclide tracer injected intraosseously reaches central circulation within a time comparable to that of intravenous injection. [7] Another study involving injection of tracers in swine in cardiac arrest showed mean time to max concentration for the tibial route was significantly longer than the sternal IO route, hypothesized to be due to proximity to central circulation. It also showed that mean dose delivered via the tibial route was 65% that of the sternal route and 53% that of the central venous route, but even in the midst of these differences, half max concentrations were reached in less than 1 minute for the tibial group. This displays that despite using the slower tibial IO route, drugs are delivered effectively and more quickly than the estimated several minutes it would take to establish an IV. [8]
Outcomes
The studies discussed so far give a convincing argument for IO access in favor of IV access in cardiac arrest, but this isn’t the whole story. We must examine clinical outcomes prior to reaching a conclusion on site of access. From 2015 through 2017 OHCA data was collected from the CARES database with the primary outcome being survival to hospital discharge in patients who received IO versus IV access for pharmacotherapy delivery and secondary outcomes including sustained ROSC and survival to hospital discharge with favorable neurologic recovery. As displayed in the table below, all outcome measures were significantly lower for IO than IV. [1]
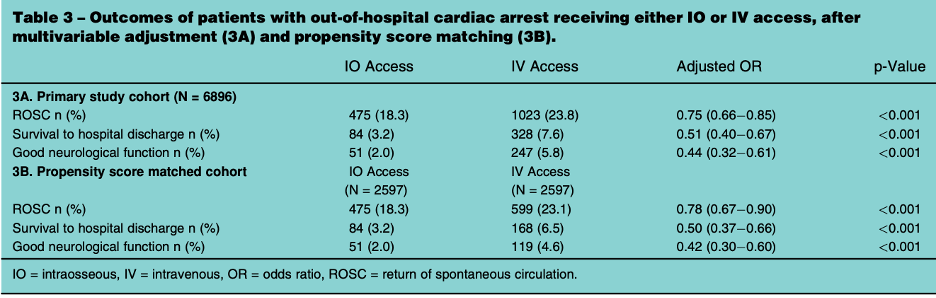
Table from Hamam et al. Resuscitation 2021 [1]
In a separate study, Clemency et al performed a retrospective chart review which showed comparable rates of ROSC in patients who received IO vs IV (19.9% vs 19.7%) access (figure below). This study showed significantly higher first attempt success with IO compared to IV. Further, first attempt success was associated with greater odds of ROSC, suggesting that IO may provide more benefit than IV as an initial site of access. [9]
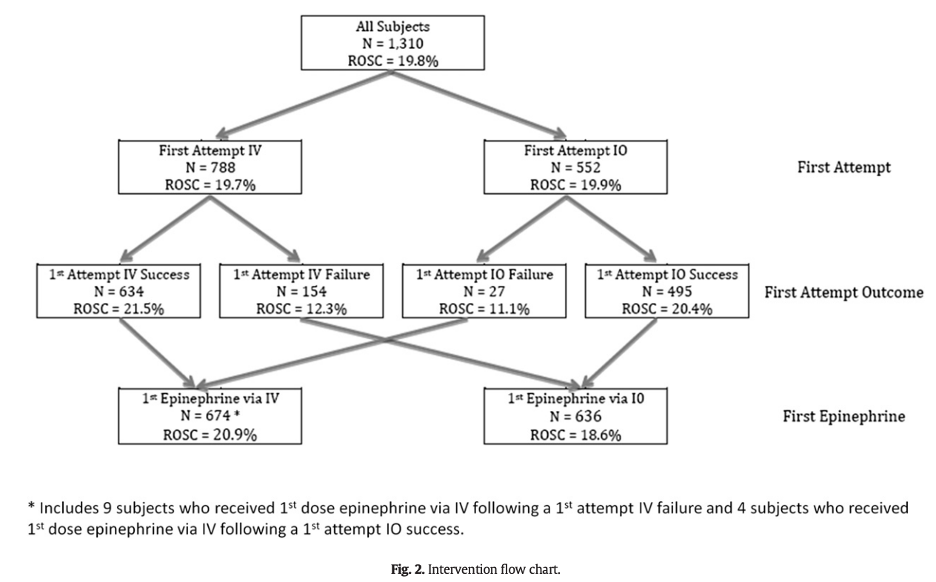
Figure from Clemency et al. American Journal of Emergency Medicine 2019 [9]
Finally, a prospective study in 2020 compared outcomes in OHCA in patients who received IV+IO access versus patients who received only IV access. In line with previously discussed studies, the IV+IO group had significantly higher success rates in obtaining access, but the study failed to show any significant differences in ROSC or survival outcomes. [3]
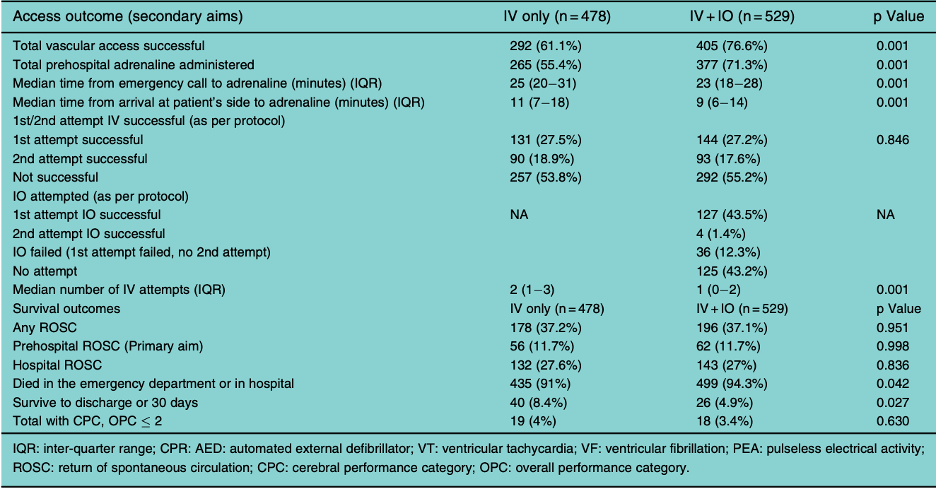
Table from Tan et al. Resuscitation 2020 [3]
Take Home Points
-
Obtaining IO access is generally quicker than obtaining IV access in cardiac arrest.
-
IO access has higher first-attempt success rates than IV access in cardiac arrest.
-
Of IO sites, the tibial IO site is associated with the least number of complications.
-
Pharmacokinetics of drugs comparable when administered IO versus IV.
-
Survival outcomes are, at best, comparable in OHCA patients who receive IO vs IV access.
-
Intraosseous vascular (IO) access is an established rapid, safe, and effective alternative for peripheral intravenous drug delivery.
-
The AHA recommends IV as preferred site of access; however, if unable to obtain IV access, then IO access is acceptable.
Future Direction
The results of the studies discussed highlight the need for randomized controlled trials to evaluate the efficacy of IO access of medication delivery during cardiac arrest. [1]
References
1. Hamam MS, Klausner HA, France J, Tang A, Swor RA, Paxton JH, O\’Neil BJ, Brent C, Neumar RW, Dunne RB, Reddi S, Miller JB. Prehospital Tibial Intraosseous Drug Administration is Associated with Reduced Survival Following Out of Hospital Cardiac Arrest: A study for the CARES Surveillance Group. Resuscitation. 2021 Oct;167:261-266. doi: 10.1016/j.resuscitation.2021.06.016. Epub 2021 Jul 5. PMID: 34237357.
2. Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, Kudenchuk PJ, Kurz MC, Lavonas EJ, Morley PT, O\’Neil BJ, Peberdy MA, Rittenberger JC, Rodriguez AJ, Sawyer KN, Berg KM; Adult Basic and Advanced Life Support Writing Group. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020 Oct 20;142(16_suppl_2):S366-S468. doi: 10.1161/CIR.0000000000000916. Epub 2020 Oct 21. PMID: 33081529.
3. Tan BKK, Chin YX, Koh ZX, Md Said NAZB, Rahmat M, Fook-Chong S, Ng YY, Ong MEH. Clinical evaluation of intravenous alone versus intravenous or intraosseous access for treatment of out-of-hospital cardiac arrest. Resuscitation. 2021 Feb;159:129-136. doi: 10.1016/j.resuscitation.2020.11.019. Epub 2020 Nov 19. PMID: 33221362.
4. Fowler R, Gallagher JV, Isaacs SM, Ossman E, Pepe P, Wayne M. The role of intraosseous vascular access in the out-of-hospital environment (resource document to NAEMSP position statement). Prehosp Emerg Care. 2007 Jan-Mar;11(1):63-6. doi: 10.1080/10903120601021036. PMID: 17169880.
5. Ross EM, Mapp J, Kharod C, Wampler DA, Velasquez C, Miramontes DA. Time to epinephrine in out-of-hospital cardiac arrest: A retrospective analysis of intraosseous versus intravenous access. Am J Disaster Med. 2016 Spring;11(2):119-123. doi: 10.5055/ajdm.2016.0230. PMID: 28102532.
6. Reades R, Studnek JR, Vandeventer S, Garrett J. Intraosseous versus intravenous vascular access during out-of-hospital cardiac arrest: a randomized controlled trial. Ann Emerg Med. 2011 Dec;58(6):509-16. doi: 10.1016/j.annemergmed.2011.07.020. PMID: 21856044.
7. Cameron JL, Fontanarosa PB, Passalaqua AM. A comparative study of peripheral to central circulation delivery times between intraosseous and intravenous injection using a radionuclide technique in normovolemic and hypovolemic canines. J Emerg Med. 1989 Mar-Apr;7(2):123-7. doi: 10.1016/0736-4679(89)90256-4. PMID: 2738371.
8. Hoskins SL, do Nascimento P Jr, Lima RM, Espana-Tenorio JM, Kramer GC. Pharmacokinetics of intraosseous and central venous drug delivery during cardiopulmonary resuscitation. Resuscitation. 2012 Jan;83(1):107-12. doi: 10.1016/j.resuscitation.2011.07.041. Epub 2011 Aug 25. PMID: 21871857.
9. Clemency B, Tanaka K, May P, Innes J, Zagroba S, Blaszak J, Hostler D, Cooney D, McGee K, Lindstrom H. Intravenous vs. intraosseous access and return of spontaneous circulation during out of hospital cardiac arrest. Am J Emerg Med. 2017 Feb;35(2):222-226. doi: 10.1016/j.ajem.2016.10.052. Epub 2016 Oct 24. PMID: 28288774.
Editing by James Li, MD EMS MEd Editor


