Author: Daniel Johnson, DO, FACEP; Assistant Professor, Department of Emergency Medicine, Life Lion EMS & Critical Care Transport, Penn State Health Milton S. Hershey Medical Center
Editors: Alex Blau, DO; Michael DeFilippo, DO, Assistant Professor of EM & EMS, WashU School of Medicine
Clinical Case
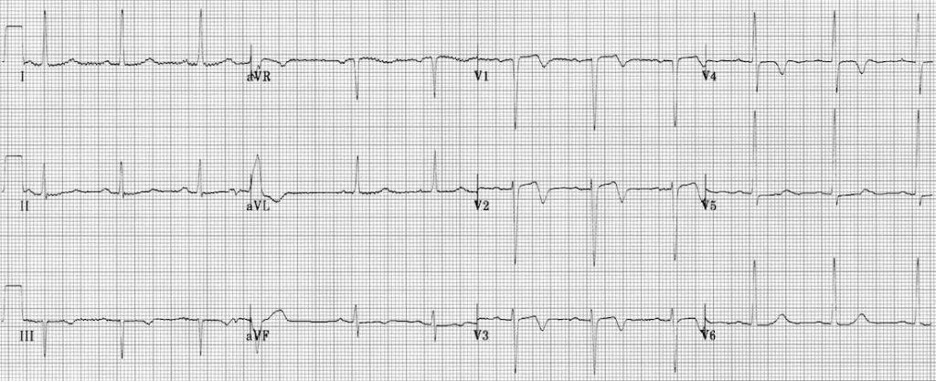
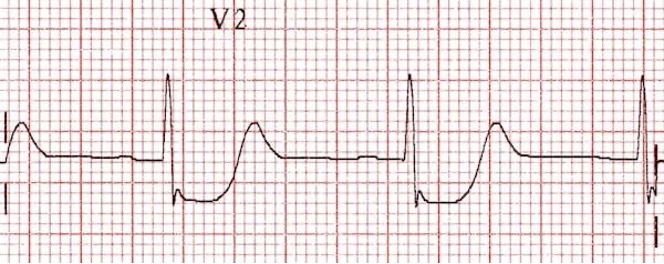
The day after a snowstorm you are working for a rural, advanced life support (ALS) agency and you are called to a 62-year-old gentleman with chest pain. He tells you that just prior to arrival, while he was shoveling snow, he developed retrosternal chest pressure radiating to his bilateral shoulders along with shortness of breath and some nausea. He called 911 and the symptoms gradually resolved as he rested. You load him in the back of your ambulance and acquire a 12-lead electrocardiogram (ECG) and it is as follows:
You are 5 minutes from a local community hospital and 45 minutes from the tertiary care center with percutaneous coronary intervention (PCI) capabilities. Which hospital do you choose?
Background
Analyzing the ECG for the presence of ST-segment elevation has become a mainstay of prehospital emergency cardiology. The subsequent diagnosis of an ST-segment elevation myocardial infarction (STEMI) sets forth a cascade of events that typically culminates in the patient being transported to hospital capable of emergent percutaneous coronary intervention (PCI). The American Heart Association recommends early PCI as a means to improve morbidity and mortality in patients suffering from STEMI1. Treatment protocols both in the field and in the hospital prioritize early acquisition of 12-lead ECGs for this very reason. While the relationship between early recognition of STEMI and improved outcomes is clear, are there other emergent cardiovascular complaints that warrant similar consideration?
In 2018, Meyers, Weingart, and Smith published “The OMI Manifesto” which shed light on the concept of a novel categorization of acute myocardial infarction2. Classically, the presence or absence of ST elevation on the ECG dictated the need for cardiac intervention. Non-ST elevation myocardial infarctions (NSTEMI) were managed medically with analgesics and antiplatelet agents , and perhaps delayed PCI. However, the notion of “STEMI equivalents” has gained traction. These are a subset of ECG findings that, while technically not meeting STEMI criteria, indicate the need for coronary intervention. The lack of a clear pathway to determine which patient’s need coronary intervention begs the question, what do we really want to know when we ask, “does the patient have ST elevation?”
Meyers et. al. introduced the concept of occlusive myocardial infarction (OMI) vs. non-occlusive myocardial infarction (NOMI) in an attempt to circumvent the pitfalls of the current STEMI vs. NSTEMI paradigm. Occlusive MI, of which STEMI would be a subset, benefit from coronary intervention, with or without classic ST elevation. Non-occlusive MI would tend to be managed medically. This speaks to the true essence of the question. Instead of asking, “which patients have ST elevation?” the question is “which patients would benefit from treatment with coronary intervention?”
There are several non-STEMI ECG findings classically associated with an acute, occlusive MI. DeWinter’s T waves, Wellen’s Syndrome, ST elevation in aVR with diffuse ST depression, isolated posterior MI, and hyperacute T-waves are some of the most common.
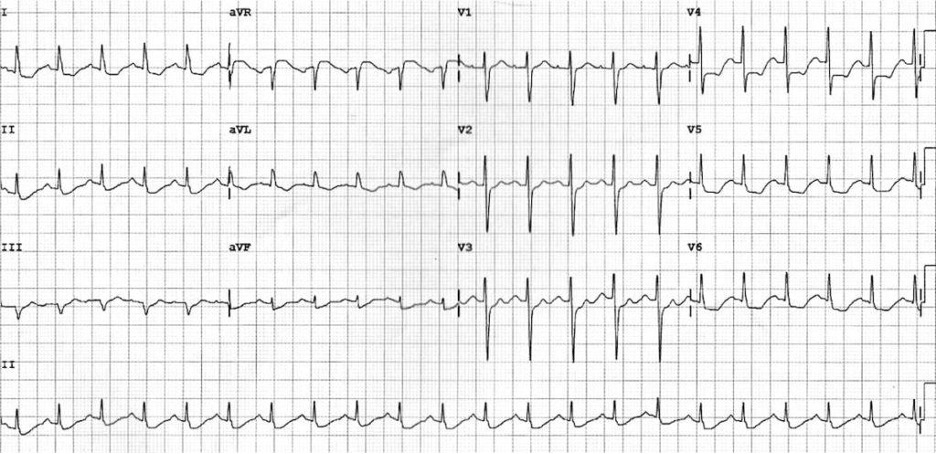
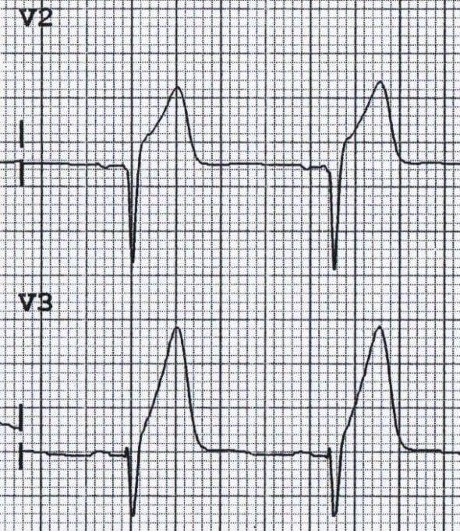
DeWinter’s T Waves

DeWinter’s T waves were first described in 2008 by Dr. Robert Jan DeWinter and are classically described as hyperacute T waves seen in the precordial leads with associated ST depression. While ST elevation is not present, these are seen in approximately 2% of acute occlusions of the left anterior descending artery. These cases may should be managed with emergent PCI.3
Wellens Syndrome
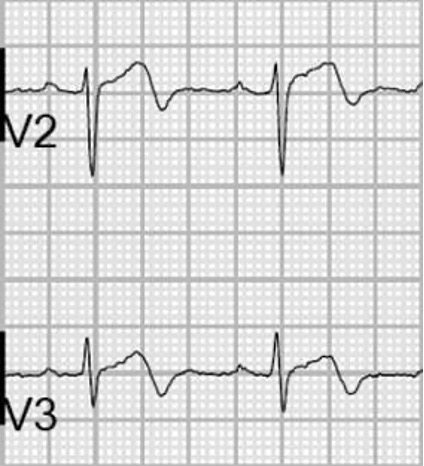
The Wellens Syndrome is the constellation of a history consistent with angina that has since resolved and ECG findings of biphasic T waves in V2 and V3. These findings are indicative of stenosis of the left anterior descending artery and require coronary intervention.4
ST elevation in aVR
The findings of ST elevation in aVR and diffuse ST depression are consistent with a diffuse mismatch of oxygen supply and demand in the myocardium. The extent of the ST depression is indicative of the global nature of the ischemia and can be associated with left main coronary artery disease, proximal left anterior descending artery stenosis, or multi-vessel coronary disease. 5 All of the above require advanced reperfusion therapy. It should be noted that this can also be seen in high stress states such as shock or immediately post-cardiac arrest.
The findings of ST elevation in aVR and diffuse ST depression are consistent with a diffuse mismatch of oxygen supply and demand in the myocardium. The extent of the ST depression is indicative of the global nature of the ischemia and can be associated with left main coronary artery disease, proximal left anterior descending artery stenosis, or multi-vessel coronary disease. 5 All of the above require advanced reperfusion therapy. It should be noted that this can also be seen in high stress states such as shock or immediately post-cardiac arrest.
Hyperacute T-waves
One of the earliest findings of an occlusive MI may be hyperacute T-waves. These are large, symmetric T waves that will correspond with coronary artery territories on the ECG.6
Isolated Posterior Myocardial Infarction
Isolated posterior MI may represent with only ST-depression in the anterior leads (V1-3).6 Posterior leads (V7-9) can be utilized to look more directly at the posterior wall of the left ventricle and, in these leads, more classic ST elevation will be noted.
So, what does this mean for EMS?
EMS has strongly adopted the notion of early STEMI recognition and transport to hospitals capable of PCI. However, as demonstrated above, there are ECG findings that could require similar treatment at centers capable of coronary intervention. Subtle, or occasionally transient, findings of Wellens Syndrome may not pique the interest of EMS clinicians the way an obvious STEMI might. These patients may therefore end up at local community hospitals with cardiac disease that needs to be treated by advanced therapies. This could precipitate worse patient outcomes and increase the burden on the EMS system when subsequent transport is required.
A recent study by Palladino et. al. examined prehospital or initial emergency department ECGs for the presence of these “STEMI equivalents” and found that approximately 4% of patients treated with emergent PCI had one of these three findings (ST elevation in aVR, De Winter T waves, and Wellens Syndrome)7. While not a large number, the impact on patient care has the potential to be significant.
Researchers are constantly questioning whether EMS interventions improve outcomes. And, if so, where is the evidence? While recognizing occlusive MI may not have the same allure of flashy therapy or new medication, the impacts cannot be overstated. The idea that EMS can ensure patients get the right care, at the right time, in the right location is critical. Timely care for patients with occlusive MI is critical and EMS is a critical link in the chain of survival.
Case Conclusion
The EMS clinicians involved in the above scenario appropriately recognized a case of Wellens Syndrome, even though the patient was now pain free. He was given aspirin and medical command was contacted to approve transport to the tertiary care center 45 minutes away and bypass the local community hospital. The patient underwent PCI to the left anterior descending artery and did well.
Acknowledgement: ECG figures for this post were found in the Life in the Fast Lane ECG Library (https://litfl.com/ecg-library/)
References
- Jneid H, Addison D, Bhatt DL, et al. 2017 AHA/ACC Clinical Performance and Quality Measures for Adults With ST-Elevation and Non–ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circulation: Cardiovascular Quality and Outcomes. 2017/10/01 2017;10(10):e000032. doi:10.1161/HCQ.0000000000000032
- Meyers H, Weingart S, Smith S. The OMI manifesto. Dr Smith’s ECG Blog http://hqmeded-ecgblogspot com/2018/04/the-omi-manifesto html. 2018;
- Winter RJd, Verouden NJW, Wellens HJJ, Wilde AAM. A New ECG Sign of Proximal LAD Occlusion. New England Journal of Medicine. 2008;359(19):2071-2073. doi:doi:10.1056/NEJMc0804737
- Rhinehardt J, Brady WJ, Perron AD, Mattu A. Electrocardiographic manifestations of Wellens’ syndrome. Am J Emerg Med. Nov 2002;20(7):638-43. doi:10.1053/ajem.2002.34800
- Yan AT, Yan RT, Kennelly BM, et al. Relationship of ST elevation in lead aVR with angiographic findings and outcome in non–ST elevation acute coronary syndromes. American Heart Journal. 2007/07/01/ 2007;154(1):71-78. doi:https://doi.org/10.1016/j.ahj.2007.03.037
- Ricci F, Martini C, Scordo DM, et al. ECG Patterns of Occlusion Myocardial Infarction: A Narrative Review. Annals of Emergency Medicine. 2025/04/01/ 2025;85(4):330-340. doi:https://doi.org/10.1016/j.annemergmed.2024.11.019
- Palladino N, Shah A, McGovern J, et al. STEMI equivalents and their incidence during EMS transport. Prehospital Emergency Care. 2022;26(1):48-54.



