Author: Robert Skinner, MD; Assistant Professor of Emergency Medicine – University of Tennessee Health Science Center
Editor: Michael DeFilippo, DO; Assistant Professor of EM and EMS – Washington University at St. Louis School of Medicine
Case: You’re on call for medical control for the day. You receive a call from a paramedic asking for orders for a 34 year old female with palpitations. Her heart rate is 180 beats per minute, and all of her other vitals are stable. Her EKG is a narrow, regular complex tachycardia consistent with supraventricular tachycardia (SVT) (or atrioventricular nodal reentry tachycardia (AVRNT) if you’re a purist). Vagal maneuvers have failed. The patient has a history of SVT and remembers feeling horrible getting that “one medicine that makes you feel like you’re going to die”; the medic asks you if they can try Diltiazem as an alternative.
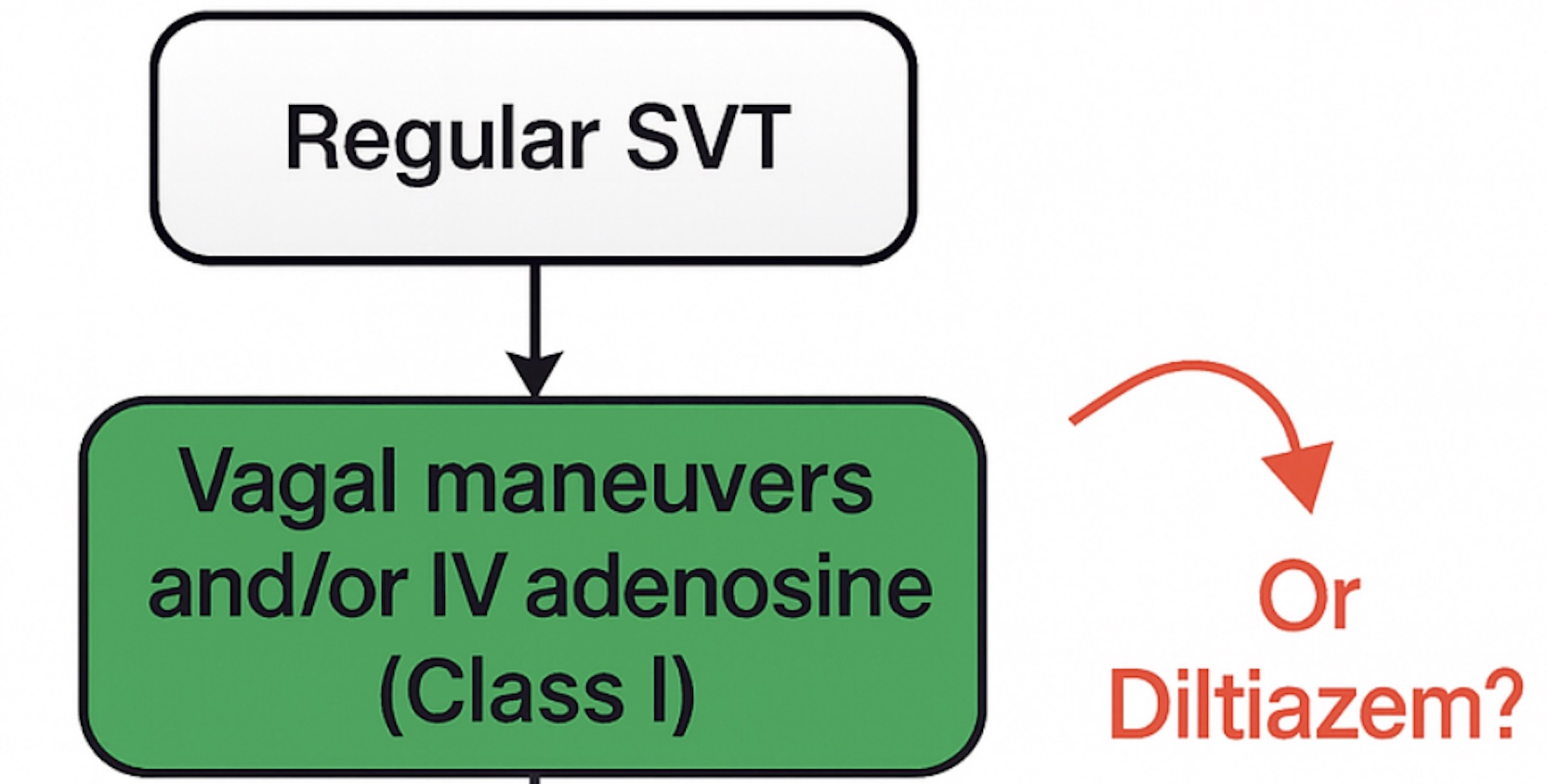
The Guidelines: The American Heart Association (AHA) defines SVT as “an umbrella term used to describe tachycardias (in rates excess over 100), the mechanism of which involves tissue from the His bundle or above” (1). The most encountered type is AVNRT, a reentrant tachycardia mediated by an accessory pathway. Treatment for SVT patients who are deemed stable are targeted at slowing conduction through the atrioventricular node (AV node). This can be done via a Valsalva maneuver in attempt to induce a vagal response. Medical treatment was classically three rounds of Adenosine, followed by Diltiazem if refractory.
Adenosine is an AV nodal blocker with a rapid onset of action and very short half-life (less than minutes). Adverse effects include nausea, sweating, numbness, and a feeling of impending doom. Other cardiac-specific adverse effects can include arrythmias, AV blocks, and prolonged periods of asystole. Contraindications for adenosine include heart block, known allergy, and active bronchospasms (2). Diltiazem is a non-dihydropyridine calcium channel blocker (CCB). Adverse effects for this medication include hypotension, bradycardia, and in some cases congestive heart failure. Contraindications include known congestive heart failure with exacerbation, wide complex tachycardias, and known allergies (3).
The current (if you call 2015 current) AHA guidelines recommend Valsalva maneuvers and/or adenosine in stable SVT. If these do not work, IV diltiazem may be considered.
…But what if we can skip the adenosine and go with diltiazem as a first line pharmacologic agent (and skip the whole impending doom thing)?
The Literature: To date, there have been multiple studies comparing adenosine and diltiazem for stable SVT:
- A 2009 study by Lim et al., compared slow infusion of calcium channel blockers to adenosine for SVT treatment in the emergency department. The study found conversion rates of 98% or greater for the CCB arm, and 86.5% for the adenosine arm. The conversion time was slower for the CCB patients (6.5-6.76 minutes vs 1.48 minutes), however the CCB was given slowly rather than a bolus. Only one patient in the CCB arm developed hypotension (4).
- An updated Cochrane review in 2017 also looked at studies comparing CCB to adenosine, finding no statistical difference in cardioversion between the two groups (5).
- A randomized control trial published in Circulation from 2021 directly compared adenosine to diltiazem. In this trial 100% of the patients converted with adenosine, vs 100% in the diltiazem group. The sample size was small, at only 52 patients. This study found no statistically significant difference in hypotension or adverse events between the two groups (6).
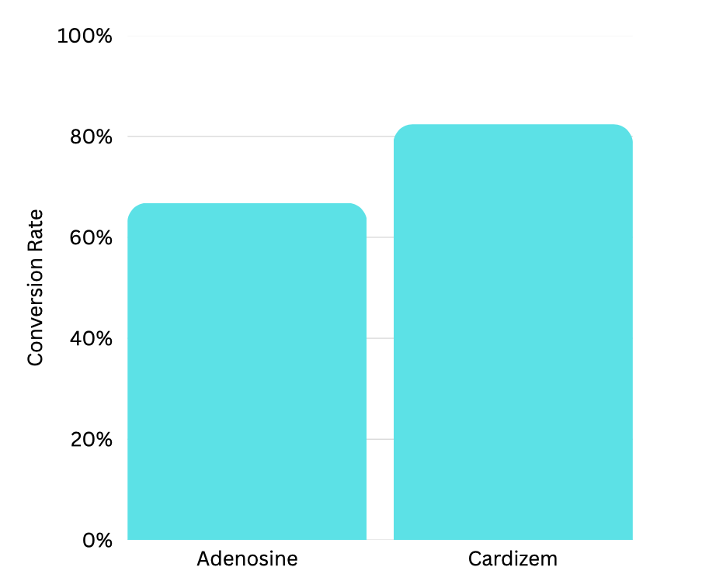
More recently, a new article, published in the Journal of Emergency Medicine in August of 2025 compared Diltiazem and Adenosine as first line medications for treatment of SVT. This was a multicenter retrospective cohort study that included 310 patients in the adenosine arm, and 34 in the Diltiazem arm. The Diltiazem arm did have a higher conversion rate (82.4%, compared to 66.8%), however the results were not statistically significant (p=0.08). The adenosine group was faster to convert out of SVT by 3 minutes (6.0 vs 3.0 mins). In cases that failed to convert with Adenosine as a monotherapy, 18 patients (35%) did convert with Diltiazem as a second agent (7).
Will this change my practice?
The literature all seems to agree that Diltiazem is a safe and effective alternative to Adenosine. No significant increases in adverse events were reported in the reviewed articles, and Diltiazem appears to be at least as effective as Adenosine. When you incorporate the additional avoidance of the patient feeling like they are going to die, Diltiazem seems like a reasonable first line option for stable SVT. Many EMS agencies are already using CCBs for rapid atrial fibrillation/flutter, and this may simplify what your crews carry on their apparatus. As with any use of CCBs, you certainly should be weary of any patients with hypotension or known heart failure.
Although the last study cited does not reach clinical statistical significance from a frequentist approach, there may indeed be noise if the same results were looked at a from a Bayesian analysis, as stated in Dr Jeff Jarvis’s fantastic EMS lighthouse podcast (8).
Sources:
- Page, R. L., Joglar, J. A., et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients with Supraventricular Tachycardia: Executive Summary. Circulation, 133(14). https://doi.org/10.1161/cir.0000000000000310
- Singh S, McKintosh R. Adenosine. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519049/
- Talreja O, Cassagnol M. Diltiazem. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532937/
- Lim SH, Anantharaman V, Teo WS, Chan YH. Slow infusion of calcium channel blockers compared with intravenous adenosine in the emergency treatment of supraventricular tachycardia. Resuscitation. 2009 May;80(5):523-8. doi: 10.1016/j.resuscitation.2009.01.017. Epub 2009 Mar 3. PMID: 19261367.
- Alabed S, Sabouni A, Providencia R, Atallah E, Qintar M, Chico TJ. Adenosine versus intravenous calcium channel antagonists for supraventricular tachycardia. Cochrane Database Syst Rev. 2017 Oct 12;10(10):CD005154. doi: 10.1002/14651858.CD005154.pub4. PMID: 29025197; PMCID: PMC6485380.
- R, N. P., Wilben, V., Kumar, V., & Kanchi, M. (2021). Abstract 10459: Adenosine versus Diltiazem in Stable Supraventricular Tachycardia Unresponsive to Vagal Maneuver. Circulation, 144(Suppl_1). https://doi.org/10.1161/circ.144.suppl_1.10459
- Lee, C. A., Morrissey, B., Chao, K., Healy, J., Ku, K., Khan, M., Kinteh, E., Shedd, A., Garrett, J., & Chou, E. H. (2025). Adenosine versus fixed-dose intravenous Bolus diltiazem on Reversing supraventricular tachycardia in the Emergency Department: a Multi-Center Cohort study. Journal of Emergency Medicine, 75, 55–64. https://doi.org/10.1016/j.jemermed.2025.05.020
- Jarvis, Jeff, Adenosine or Diltiazem for SVT, The EMS Lighthouse Project, Episode 99, FlightBridgeED, 12 July 2025. https://flightbridgeed.com/emslhp-podcast/



