by Richard T. Benson II, MD, Joseph Grover, MD, Jane Brice, MD, MPH
Clinical Scenario:
EMS is dispatched to a possible stroke patient whose last seen normal time was 1.5 hours prior to dispatch. The patient lives 15 minutes from a primary stroke center and 45 minutes from a comprehensive stroke center. The patient has complete hemiparesis on the right, aphasia, with facial droop. Which facility should the patient be transported to via EMS?
Literature Review:
Stroke is the fifth leading cause of death in the United States and is a major cause of adult disability [1]. About 800,000 people in the United States have a stroke each year; and on average, one American dies from a stroke every 4 minutes [1,2]. Most strokes (85%) are ischemic, meaning an artery that supplies oxygen-rich blood to the brain becomes blocked. There are also hemorrhagic strokes (15%) where an artery in the brain leaks out blood or completely ruptures. An acute stroke represents a neurologic emergency that requires time-dependent treatments to mitigate the insult. Over the past 20 years, EMS has played a vital role in the triage and management of stroke. In 1995 an article published in the New England Journal of Medicine (NEJM) revolutionized the care of stroke patients when it demonstrated the benefit of tissue plasminogen activator (tPA) in the treatment of acute ischemic stroke [3]. Nationally, this led to the creation of Primary stroke centers – facilities capable of administering systemic tPA. Because of this, many EMS systems created specific destination plans, with the goal of getting possible stroke patients to a Primary stroke center as fast as possible. In addition, stroke scales were developed to aid providers in the early recognition of stroke. Ultimately, providers were able to appropriately triage possible stroke patients, transporting them to capable facilities, and provide pre-notification to those facilities or “Code strokes.” This decreased in-hospital delays and led to quicker dispositions and treatments. Ekundayo et al demonstrated that EMS play a major role in stroke management, transporting the majority of stroke patients (63.7%), as well as, those stroke patients with the higher stroke severity scores [4]. In 2015, almost 20 years after the FDA approved tPA for the management of stroke, the NEJM published five studies which demonstrated the superiority of endovascular treatment for Large Vessel Occlusion (LVO) strokes over the standard treatment of tPA alone. 5-9 It should be noted, that approximately 70% of the patients in the mentioned trials received intravenous (IV) tPA, in addition to endovascular treatment. This led to the creation of Comprehensive stroke centers – facilities capable to administering IV tPA and administering intra-arterial thrombolysis. These studies provide compelling evidence to support transporting LVO stroke patients to a comprehensive stroke center over primary stroke center, if available. With EMS transporting the majority of stroke patients and those patients with the highest stroke severity scores, this fundamental change in the management of stroke patients with LVOs should have a significant impact on how EMS systems triage and transport stroke patients.
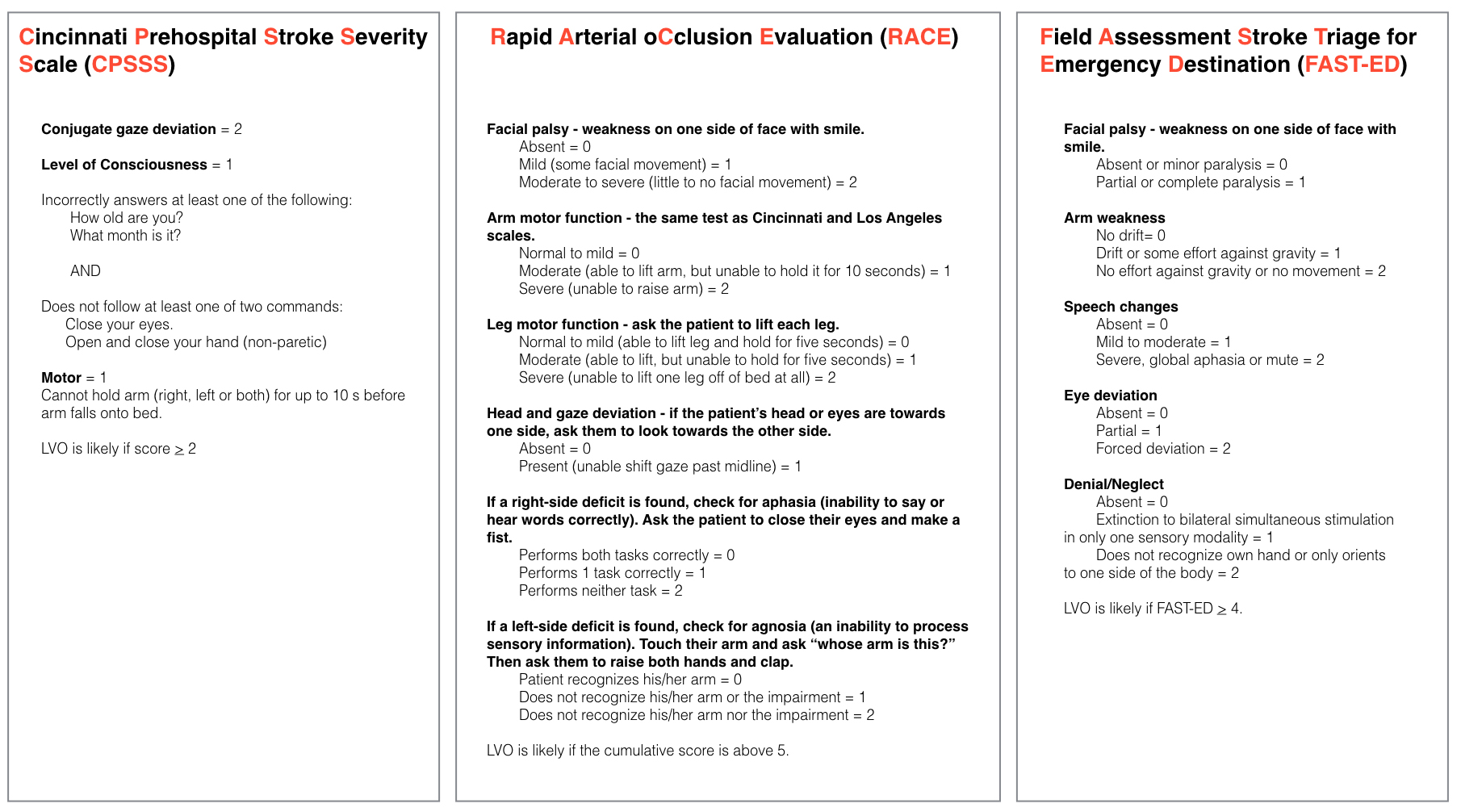
The greatest difficulty for current EMS systems is differentiating LVO stroke patients from the standard stroke patient in the hopes of getting them to the most appropriate stroke center. Many EMS systems utilize either the Cincinnati Prehospital Stroke Scale (CPSS) or the Los Angeles Prehospital Stroke Scale (LAPSS) for their stroke recognition. Multiple studies have been done looking at these scales with the results showing varying sensitivities with relatively low specificities [10-11]. None of these current scales differentiate a LVO from a stroke and therefore could not aid providers in making a decision to bypass a primary stroke center for a comprehensive stroke center. To address this need newer scales have been developed to aid providers in this regard. The simplest scale utilizes severe hemiparesis as their sole criteria, and found 26.7% had an LVO that was treated with thrombectomy [12]. Other scales have been developed including the Cincinnati Prehospital Stroke Severity Scale (CPSSS), RACE scale, and the FAST-ED scale which show promising results in differentiating LVO from a standard stroke [13,14,15]. The associated time delays of transferring a patient from one facility to the other would likely prevent patients from receiving endovascular therapy and therefore every effort must be made to accurately triage these patients to the most appropriate facility first [16].
Take Home Points:

Over the past 20 years, the early recognition and treatment of strokes have come a long way, with the help of stroke scales and tPA administration. EMS has always been a key component in effective and timely management of these patients. Emerging evidence demonstrates the superiority of combined systemic IV tPA with endovascular treatment in patients with LVO over systemic tPA alone, challenging EMS systems to develop sensitive screening tools for LVO and updated destination plans.
References
1. Kochanek KD, Xu JQ, Murphy SL, Arias E. Mortality in the United States, 2013. NCHS Data Brief, No. 178. Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention, US Dept. of Health and Human Services; 2014.
2. Mozzafarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015:e29–322.
3. Tissue plasminogen activator for acute ischemic stroke. the national institute of neurological disorders and stroke rt-PA stroke study group. N Engl J Med. 1995;333(24):1581-1587.
4. Ekundayo OJ, Saver JL, Fonarow GC, et al. Patterns of emergency medical services use and its association with timely stroke treatment: Findings from get with the guidelines-stroke. Circ Cardiovasc Qual Outcomes. 2013;6(3):262-269
5. Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20.
6. Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-1018.
7. Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030.
8. Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296-2306.
9. Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372(24):2285-2295.
10. Asimos AW, Ward S, Brice JH, Rosamond WD, Goldstein LB, Studnek J. Out-of-hospital stroke screen accuracy in a state with an emergency medical services protocol for routing patients to acute stroke centers. Ann Emerg Med. 2014;64(5):509-515.
11. Oostema JA, Konen J, Chassee T, Nasiri M, Reeves MJ. Clinical predictors of accurate prehospital stroke recognition. Stroke. 2015;46(6):1513-1517.
12. Gupta R, Manuel M, Owada K, et al. Severe hemiparesis as a prehospital tool to triage stroke severity: A pilot study to assess diagnostic accuracy and treatment times. J Neurointerv Surg. 2015.
13. Katz BS, McMullan JT, Sucharew H, Adeoye O, Broderick JP. Design and validation of a prehospital scale to predict stroke severity: Cincinnati prehospital stroke severity scale. Stroke. 2015;46(6):1508-1512.
14. Perez de la Ossa N, Carrera D, Gorchs M, et al. Design and validation of a prehospital stroke scale to predict large arterial occlusion: The rapid arterial occlusion evaluation scale. Stroke. 2014;45(1):87-91.
15. Prabhakaran S, Ward E, John S, et al. Transfer delay is a major factor limiting the use of intra-arterial treatment in acute ischemic stroke. Stroke. 2011;42(6):1626-1630.
16. Lima FO, Silva GS, Furie KL, et al. Field Assessment Stroke Triage for Emergency Destination: A Simple and Accurate Prehospital Scale to Detect Large Vessel Occlusion Strokes. Stroke. 2016 Jun 30
EMS MEd Editor: Maia Dorsett



