by Melody Glenn, MD
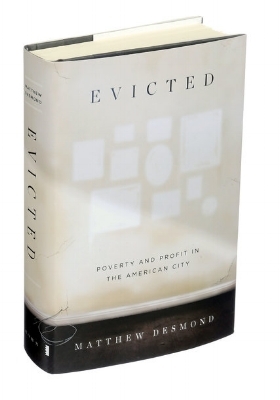
Perhaps the success of Harvard sociologist Matthew Desmond’s Evicted, Poverty and Profit in the American City, lies in its engaging style, reading more like a page-turning novel and less like an academic analysis. Through following the ups and downs of its colorful characters, we realize the profound impact that stable housing has on individuals, communities, and their health. Although the setting is in Milwaukee, the lessons are transferable, as unaffordable housing is a problem nationwide.
From the individuals’ narratives, we see how easy it is to crash to the bottom if you are poor; there is no safety net to catch you. In the first pages of the book, Arleen and her two boys are evicted after a man breaks down their door. There is little incentive for landlords in poor neighborhoods to pay for costly repairs, as they know that the market for low-cost housing far outstrips demand. After a family has an eviction on their record, they have even less bargaining power, and are thus more likely to be forced into substandard housing conditions, as are Arleen and her boys when they subsequently rent a decrepit $550/month apartment in one of the worst neighborhoods in American’s fourth-poorest city. The rent takes 88% of Arleen’s monthly income, which is not uncommon. The majority of poor renting families spend half of their income on housing, which is far above the traditionally recommended 30%. Given those numbers, perhaps it isn’t so surprising that 1 in 8 renters experienced a forced move between 2009 and 2011 in Milwaukee, and that similar numbers are seen nationwide.
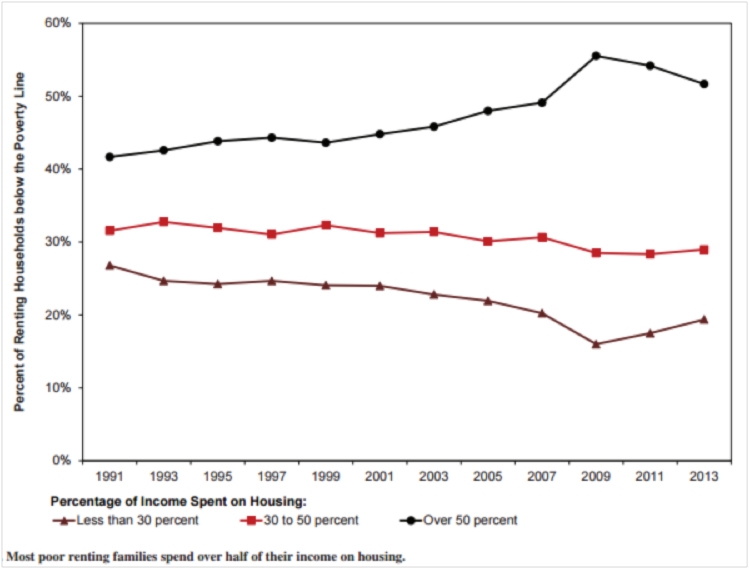
Image Source: Desmond, M. Unaffordable America: Poverty, housing, and eviction. Fast Focus, University of Wisconsin-Madison. 2015; 22. http://www.irp.wisc.edu/publications/fastfocus/pdfs/FF22-2015.pdf
Arleen and her boys are again evicted, and Arleen attempts, unsuccessfully, to fight her eviction at eviction court. As people have no right to an attorney in civil court, 90% of tenants in housing courts nationwide do not have attorneys, whereas 90% of landlords do [1]. Looking around her, Arleen notices that the other tenants are predominantly black females. Matthew Desmond writes, “If incarceration had come to define the lives of men from impoverished black neighborhoods, eviction was shaping the lives of women. Poor black men were locked up. Poor black women were locked out.” [1]
Later in the book, Arleen and her boys are again evicted, but this time via the nuisance property ordinance. After their roommate calls 911 in response to a domestic disturbance in the unit upstairs, the police contact the landlord, informing her that she will be responsible for a fine or jail time if there are any further “nuisance activities” on her property, and requiring her to submit a plan as to how she will “abate the nuisance activities.” Her initial plan was not accepted by the police department, but the 2nd plan, eviction of the tenants, was.
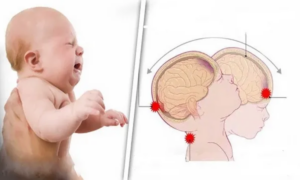
Nationwide, the majority of nuisance citations are related to domestic violence calls, which discourages victims from calling 911 [1]. A study by Rollins et al suggested that among victims of intimate partner violence, evictions and housing instability were predictors of PTSD, depression, increased work/school absence, and increased ED/hospital use [2]. Additionally, black tenants are more likely to receive nuisance citations, and thus evictions, than are their white counterparts. In black neighborhoods, 1 in 16 eligible properties receive a citation, compared to 1 in 41 in white neighborhoods [1].
Arleen and her boys move into a shelter, and within the span of 2 months, she applies to, and is rejected by, 89 prospective apartments. This is likely secondary to both her eviction record and the fact that she has children. The Fair Housing Act of 1968 did not consider families with children a protected class, so many units charged children-damage deposits and monthly surcharges. In 1988, housing discrimination against children and families was outlawed, but the practice continued. In as many as 7 in 10 housing searches, families with children were turned away [1].
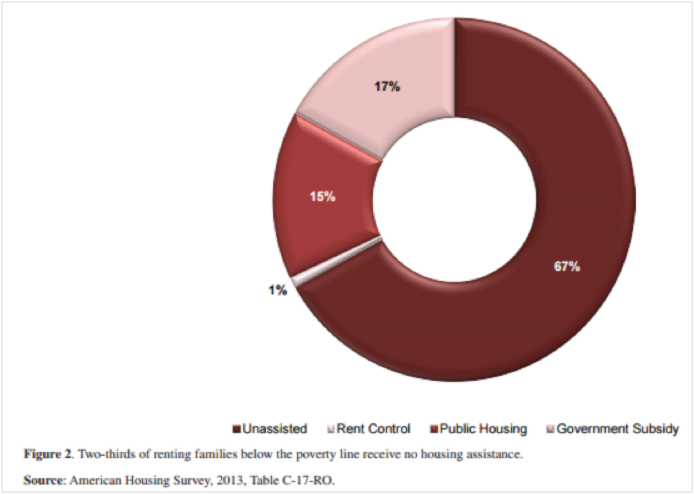
Image Source: Desmond, M. Unaffordable America: Poverty, housing, and eviction. Fast Focus, University of Wisconsin-Madison. 2015; 22. http://www.irp.wisc.edu/publications/fastfocus/pdfs/FF22-2015.pdf
Arleen’s eviction is also a strike against her when applying for public housing assistance. Even if she qualified, ¾ of families in America who qualify for assistance receive nothing. In Milwaukee, the list for rental assistance was frozen [1]. In some cities, the wait for public housing is counted in decades.
Evictions have dramatic, negative effects on people’s jobs and children’s educational trajectories. Arleen’s son Jori attends 5 different schools between the 7th and 8th grades, and her son Jafaris starts to show signs of anger issues and learning disabilities, which is not uncommon in children who are experience housing instability. Multiple studies have shown that evictions and housing instability increase rates of depression, suicide attempts, decreased medication compliance, gaps in health insurance, and even low birth weights [3-9].

James Baldwin (Image Source: Wiki Commons)
Although Arleen is not working, many of the other characters in the book are, or were, until they were evicted. Desmond notes that workers who involuntarily lost their housing were roughly 20 percent more likely subsequently lose their jobs, compared to similar workers who did not [10]. [GM2] As eviction leads to so many destabilizing, downstream effects that place individuals and their communities on a downward trajectory, Desmond argues that eviction is a cause, not just a condition, of poverty. As James Baldwin wrote in Fifth Avenue, Uptown “Anyone who has ever struggled with poverty knows how extremely expensive it is to be poor; and if one is a member of a captive population, economically speaking, one\’s feet have simply been placed on the treadmill forever.” [11]
On April 4th, our interdisciplinary book club met at The Laughing Monk Brewery to discuss the relevance of Desmond’s work to our communities and professional practice here in the Bay Area. In the Mission neighborhood, where many of us work at Zuckerberg San Francisco General Hospital, the Anti-Eviction Mapping Project documents that there have been 908 evictions since 2011 [12]. They also have a map of all evictions in San Francisco, stratified by type, which shows that nuisance evictions are the 3rd most common cause.

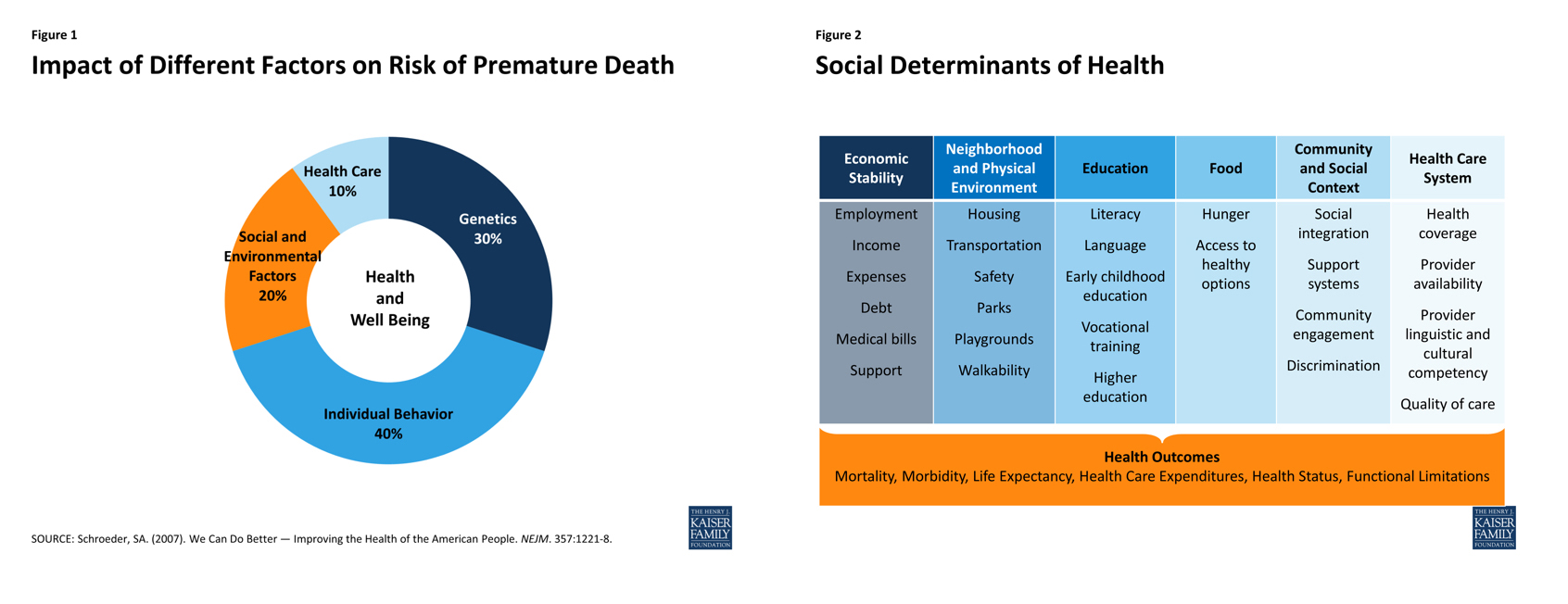
The statistics and arguments in Desmond’s book support the theory that of all the social determinants of health, housing insecurity may be one of the most detrimental. For those of you who may be new to the term, “social determinants of health,” the WHO defines them as the forces that lead to health inequities and are beyond the span of control of the individual, and include education, race, neighborhood, and labor and housing markets [13]. According to a study by Galea et al, social factors are attributable to more deaths in the US than are acute MI’s, CVA, and lung cancer [14].
In San Francisco, the Department of Public Health began to treat housing instability as a public health issue. They saw that many of their highest users and those who were severely disabled often did not qualify for low-income housing, so they opened their own housing facilities [15]. They obtained federal funds dedicated for initiatives based on Housing First, which is an approach that reduces barriers, such as preconditions of abstinence, to housing, under the belief that addiction and mental health issues will improve after individuals attain a safe living situation. In 2009, JAMA published an article showing that implementation of a Housing First intervention for chronically homeless individuals with severe alcohol problems and high service use lead to a decrease in health care and public service use, saving an average of $2,449 per person after accounting for housing program costs [16].
Even with the involvement of local government, there still isn’t enough low-cost or subsidized housing to meet the demand. As Dr. Barry Zevin, the medical director of the San Francisco Street Medicine & Shelter Health Team, stated, “We are trying to find local solutions to a national problem.” That being said, it does seem like San Francisco faces some additional challenges due to particularly high rents and limited space. According to Trulia, the median price of a one-bedroom apartment in SF was just shy of $3,000 month in October of 2016. According to an article in Quartz, in 2005, the Bay Area added 64,000 in jobs but only 5,000 new homes were built[17. In San Francisco, there are an estimated 6,000- 7,000 homeless people in the city every night, and public health records suggest that a whopping 13,000 – 14,000 people experience homelessness at some point during the year [18]. As Dr. Zevin summarizes, we have a “liberal ethos that crashes up against incredible disparity.”
April Bassett, a captain & community paramedic with the San Francisco Fire Department who focuses on improving care for the city’s frequent 911-users, addressed the myth of the existence of a strong safety net: “Let’s talk about how hard it is to get benefits in the city.” In order to get social services, you need an ID. In order to get an ID mailed to you, you need an address. Furthermore, if you have an untreated psychiatric condition, you may be too disorganized to complete the multi-step process of obtaining an ID. Dr. Zevin, much like April and Desmond, has learned just “how hard the gains are, yet how easy and multiplying the losses are.”
As an emergency physician in the Bay Area, I have come to see how housing instability affects the health of my patients, and the effectiveness (or lack thereof) of my interventions. Diabetics with DKA because their insulin was stolen while living on the street, patients whose blood pressure was sky-high because their medications were left behind in their old house, patients with severe asthma exacerbations because they did not have enough money left over to pay for their inhaler even after working two jobs, patients whose chronic venous stasis ulcers continue to worsen because they don’t have a clean place to wash and change their dressings. My treatments just feel like a Band-Aid that will become ripped off as soon as they leave the ED. I imagine I’ll see them again in a few days, and the data supports this; a study by the Agency for Healthcare Research and Quality found that ED visits are 9-12 times higher among homeless men and women [19].
As medics and emergency medicine practitioners, what can we do? Dr. Zevin stressed the importance of simply documenting our patients’ housing status and if they have evidence of psychosis. It also helps us better meet our patients where they are, and adds perspective and continuity to future encounters (i.e., is the homelessness or mental illness new or is it years old?). Then we can better address “their barriers to care and the system gaps.” Maggie Roberts JD, a civil rights attorney who often advocates for those with disabilities, emphasizes the value of this simple task; if these patients ever try to apply for benefits, such documentation is hugely important.
Amber Quelvog, an ER nurse at San Francisco General Hospital, suggested that the nurse in triage check a box in the chart if a patient were currently homeless, and then the patient’s chart could be forwarded to one of the public health clinics (if such a transfer of information were made more systematic and HIPAA compliant) As Dr. Zevin asserts, “If someone is on [our] radar, there is a better chance that they will get to what they need.”
We also have to decide whether or not we think housing is a human right, and if so, support policies and regulations that increase access to housing. Matthew Desmond suggests making the current voucher system more efficient and expanding its availability to include more people. Josh Seim, a PhD candidate in sociology at UC Berkeley, thinks the solution needs to involve more public housing.
As EMS providers, I believe that this is in our wheelhouse. One direct way that we can work to address the negative health effects of housing instability is through community paramedicine initiatives that better plug people into the care they need — whether that is social services, primary care, mental health, or addiction programs. In San Francisco, ED providers and field medics refer vulnerable, frequent-user patients to their EMS-6 Community Paramedicine team [20]. April, or one of the other community paramedics, and a social worker then go to the field to meet the patient wherever they are, from a tent on the sidewalk to a hospital bed at UCSF, and start to address their individual barriers to care. Often times, this centers around housing instability, so the team helps their clients fill out the necessary shelter or supportive housing applications, or gets them into medical detox programs that can better help them in this transition. They help their patients better navigate the system. If your EMS system doesn’t have a community paramedicine program, there are other ways to have an effect, such as medic-led patient referrals to social services organizations, or EMS Agency support.
Dr. Zevin tries to end the discussion with an uplifting tone, “The resilience of the people I see is amazing. The things that would kill me do not kill them. The things that would destroy my spirit mostly do not destroy the spirit of my patients. Their material circumstances are horrible, and the outlook is pretty bleak. But people keep trying. And they appreciate even the little things we can do for them. I need to hold onto that, or things look pretty bleak. These are consequences of national problems, not local problems, although there are strange local bits to this. Donate. Understand the victories we have gotten. That helps me keep going.”

Image Source: Melody Glenn, personal photo
Take home points:
Homelessness and housing instability have negative health outcomes
Homelessness is associated with a higher frequency of ER visits
Document homelessness and abnormalities in your patients’ psychiatric exams
EMS can help refer patients to needed social services and address barriers to care
References
1. Desmond, Matthew. Evicted: Poverty and Profit in the American City. 2016.
2. Rollins C, Glass NE, Perrin NA, Billhardt KA, Clough A, Barnes K, HansonGC, Bloom TL. Housing instability is a strong predictor of poor health outcomes as level of danger in abusive relationship: findings from the SHARE study. J Interpers Violence. 2012 Mar; 27(4): 623-43.
3. Bolívar Muñoz J1, Bernal Solano M2, Mateo Rodríguez I3, Daponte Codina A3, Escudero Espinosa C4, Sánchez Cantalejo C4, González Usera I5, Robles Ortega H5, Mata Martín JL5, Fernández Santaella MC5, Vila Castellar J5. The health of adults undergoing an eviction process]. Gac Sanit. 2016 Jan-Feb;30(1):4-10. [Article in Spanish]
4. Burgard SA1, Seefeldt KS, Zelner S.Housing instability and health: findings from the Michigan Recession and Recovery Study. Soc Sci Med. 2012 Dec;75(12):2215-24.
5. Carrion BV1, Earnshaw VA, Kershaw T, Lewis JB, Stasko EC, Tobin JN, Ickovics JR. Housing instability and birth weight among young urban mothers.J Urban Health. 2015 Feb;92(1):1-9. doi: 10.1007/s11524-014-9913-4.
6. Carroll A1, Corman H2, Curtis MA3, Noonan K4, Reichman NE5. Housing Instability and Children\’s Health Insurance Gaps. Acad Pediatr. 2017 Feb 20. pii: S1876-2859(17)30062-1.
7. Fowler KA1, Gladden RM, Vagi KJ, Barnes J, Frazier L. Increase in suicides associated with home eviction and foreclosure during the US housing crisis: findings from 16 National Violent Death Reporting System States, 2005-2010. Am J Public Health. 2015 Feb;105(2):311-6.
8. Rojas, Y. Evictions and short-term all-cause mortality: a 3-year follow-up study of a middle-aged Swedish population. Int J Public Health. 2017 Apr;62(3):343-351. 9. Rojas Y1, Stenberg SÅ1. Evictions and suicide: a follow-up study of almost 22,000 Swedish households in the wake of the global financial crisis. J Epidemiol Community Health. 2016 Apr;70(4):409-13.
9. Vásquez-Vera H1, Palència L2, Magna I3, Mena C3, Neira J3, Borrell C4. The threat of home eviction and its effects on health through the equity lens: A systematic review. Soc Sci Med. 2017 Feb;175:199-208.
10. Desmond, M. Unaffordable America: Poverty, housing, and eviction. Fast Focus, University of Wisconsin-Madison. 2015; 22. http://www.irp.wisc.edu/publications/fastfocus/pdfs/FF22-2015.pdf
11. Baldwin, J. Firth Avenue, Uptown. Esquire. July 1960. http://www.esquire.com/news-politics/a3638/fifth-avenue-uptown/
12. http://www.antievictionmap.com/
13. http://www.who.int/social_determinants/en/
14. Galea S et.al. Estimated Deaths Attributable to Social Factors in the US. AJPH:June 16,2011;eprint.
15. per Barry Zevin, MD
16. Larimer, Mary E.; Malone, Daniel K.; Garner, Michelle D.; Atkins, David C.; Burlingham, Bonnie; Lonczak, Heather S.; Tanzer, Kenneth; Ginzler, Joshua; Clifasefi, Seema L.; Hobson, William G.; Marlatt, G. Alan (1 April 2009). “Health Care and Public Service Use and Costs Before and After Provision of Housing for Chronically Homeless Persons with Severe Alcohol Problems”. JAMA. 301 (13): 1349–57.
18. http://dhsh.sfgov.org/research-reports/san-francisco-homeless-point-in-time-count-reports/
19. Hwang SW, Henderson MJ. Health Care Utilization in Homeless People: Translating Research into Policy and Practice. Agency for Healthcare Research and Quality Working Paper No. 10002, October 2010, http://gold.ahrq.gov.
20. http://www.sfchronicle.com/bayarea/article/Emergency-responder-to-be-honored-for-treating-6828232.php