TL;DR
-
TXA is used to stabilize clots by preventing fibrinolysis
-
Dose: 1g over 10 minutes, then 1g over 8 hours
-
CRASH-2 has shown an improvement in survival
-
Even greater improvement if administered within 3 hours (earlier is better!)
-
-
CRASH-3 has shown mortality improvement in mild-moderate isolated head trauma (GCS 9-15)
-
TXA rate of vascular occlusive events = placebo rate of vascular occlusive events
-
Consider adding TXA to pre-hospital protocols as an adjunct to stop the bleed
The Articles:
Background:
If you recall the clotting cascade, the end of the process involves the breakdown of clots (also known as fibrinolysis), through the activation of plasminogen to plasmin. Tranexamic acid (TXA) is a synthetic form of lysine, an amino acid. TXA is used to block fibrinolysis by attaching to plasminogen and blocking the fibrin binding site, preventing the formation of plasmin. Historically, TXA has been used in the operating room to stabilize already formed clots to prevent worsening bleeding.
Naturally, the next step is to see whether the drug can prevent bleeding in other settings besides the O.R. In this article bite, we will discuss CRASH-2 and CRASH-3 – two large studies on the efficacy of TXA in trauma.
CRASH-2 Methods:
CRASH-2 was a randomized double-blinded control study involving 20,211 patients across 274 hospitals in 40 countries. The study group had the following inclusion criteria:
-
Adult trauma patients
-
Significant hemorrhage
-
Hypotension with systolic blood pressure < 90 mmHg and/or
-
Tachycardia with heart rate > 110
-
-
At risk for significant hemorrhage
-
Within 8 hour of injury
In addition, the study excluded cases where giving TXA was the obvious clinical choice. This exclusion allowed the researchers to focus on patient care guided by the uncertainty principle (ie. when the risk/benefit was less clear). Patients were randomized to either receive normal saline or TXA 1g infused over 10 minutes, then infusion of 1g over 8 hours.
The primary outcome was death in hospital within 4 weeks (28 days) of injury. This was then broken down by cause of death:
-
All cause mortality
-
Bleeding
-
Vascular occlusion (myocardial infarction, stroke, PE)
-
Multiorgan failure
-
Head injury
-
Other
Primary outcomes were further stratified by time since injury, systolic BP, GCS, and type of injury in subgroup analysis.
Secondary outcomes included:
-
Vascular occlusive events (myocardial infarction, stroke, PE, and DVT)
-
Need for surgical intervention (neurosurgical, thoracic, abdominal, and pelvic)
-
Receipt of blood transfusion
-
Units of blood products transfused
-
Level of disability (measured with the 5-point Modified Oxford Handicap Scale)
CRASH-2 Key Results:
A total of 10,060 patients were analyzed in the TXA group and 10,067 patients were analyzed in the placebo group. The primary outcomes are illustrated in the following table (Table 2 in Crash-2).
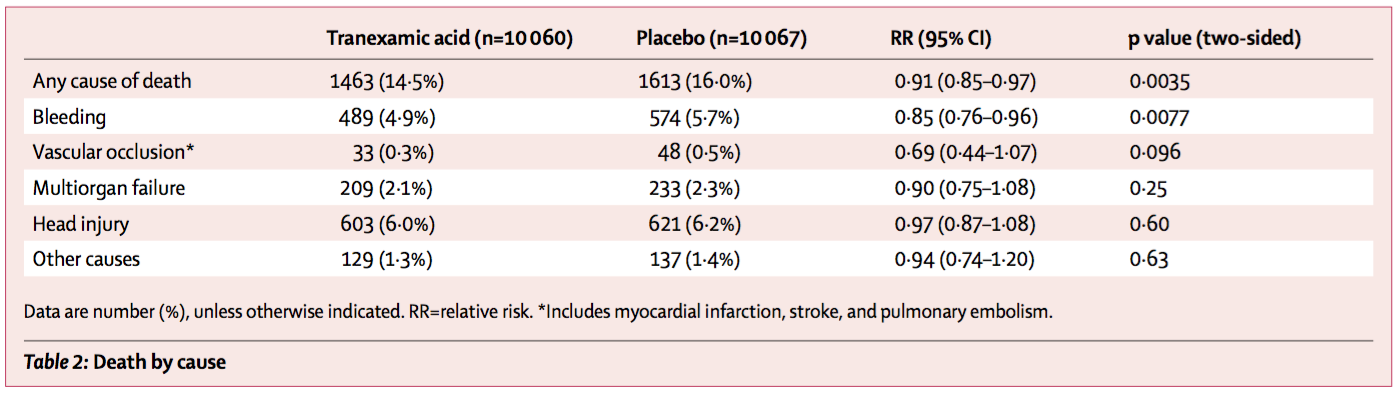
CRASH-2 Primary Outcomes
Essentially, there was:
-
A decrease in any cause of death in TXA (14.5%) versus placebo (16.0%)
-
A decrease in death by bleeding in TXA (4.9%) versus placebo (5.7%)
-
No noted difference in deaths from multiorgan failure, head injury, or other causes.
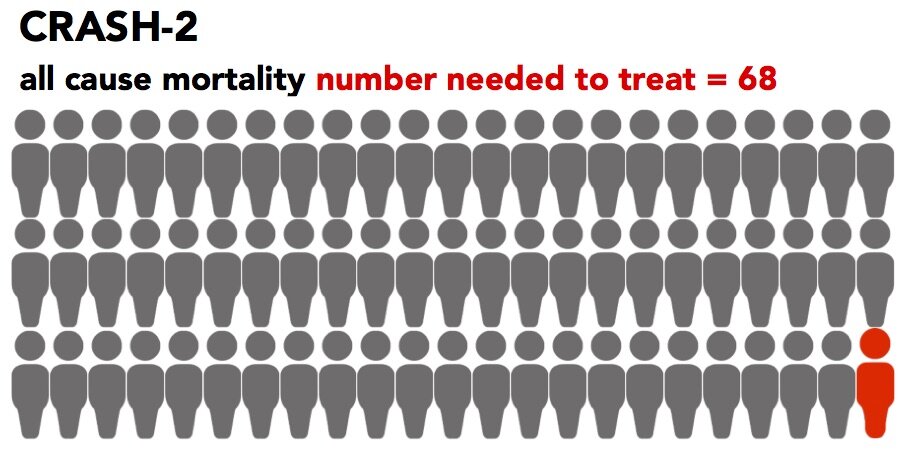
To put this into perspective, the number needed to treat (NNT) is 68, meaning in order to save one life from any cause of death, you need to treat 68 patients with TXA. In order to save one life from death by bleeding, you need to treat 119 patients.
Importantly, in a secondary analysis of the data, they found that early administration reduced mortality even more!
-
Within 1 hour: 5.3% (TXA) vs. 7.7% (placebo)
-
Between 1-3 hours: 4.8% (TXA) vs. 6.1% (placebo)
As for the secondary outcomes, there was:
-
No difference in vascular occlusive events
-
No difference in need for transfusion or surgery
-
Statistically significant increase in patients discharged with no symptoms in the TXA group
Now before we dive into the takeaways, let’s quickly talk about CRASH-3…
CRASH-3 Methods:
CRASH-3 likewise was a multicenter double-blinded, randomized, placebo-controlled trial involving 12,737 patients with the following inclusion criteria:
-
Adults age ≥ 18 years
-
Within 3 hours of injury
-
No major extracranial bleeding
-
GCS ≤ 12 or evidence of intracranial bleeding on CT scan
Likewise, primary outcome was death at 28 days, with secondary outcomes of complications, need for surgical intervention, disability, etc.
CRASH-3 Key Results:
CRASH-3 was able to show mortality benefit only in patients with mild to moderate head injury (GCS 9-15) with mortality of 5.8% in the TXA group versus 7.5% in the placebo group. To put it more practically, you would need to give 61 patients TXA with mild to moderate head injury in order to save 1 patient (NNT = 61). However, CRASH-3 was unfortunately not able to show a statistically significant reduction in mortality in all patient or a difference in disability. What is important, though, is that CRASH-3, like CRASH-2, was unable to show any increase in complications, therefore highlighting the safety of TXA.
Takeaways:
In these two incredibly large studies in a very heterogeneous population group, TXA has been shown to improve overall patient survival in trauma and, in a specific patient group, isolated head trauma. However, it’s important to remember that these improvements are modest at best. For all trauma, we are looking at a number needed to treat of 68 and for head trauma specifically, you are looking at a number needed to treat of 61, but only in mild to moderate head trauma.
So is it worth it? It probably depends! TXA in general is relatively inexpensive and very safe. Given that for our very sick trauma patients, there aren’t a lot of options other than to take them to the operating room faster or to drive the ambulance faster, it is incredibly reasonable to incorporate TXA into your practice.
Implications for EMS:
While trauma care in EMS has vastly improved in the United States, there is still room for improvement. As CRASH-2 and CRASH-3 have demonstrated, TXA is not only both efficacious and safe in trauma patients, but leads to even better outcomes when given as soon a possible after time of injury. As the first point of medical contact for our trauma patients, incorporation of TXA to EMS protocols can shorten the time to administration of TXA, especially in rural communities with long transport times, therefore improving patient survival.
Article Bites Summary by Alison Leung, MD (@alisonkyleung)
EMS MEd Editor: Alicia Buck, MD