by Sahar Morkos El-Hayek, MD
EMS MEd Editor Maia Dorsett, MD PhD (@maiadorsett)
This past summer, the results of the REALTY-AHF (Registry Focused on Very Early Presentation and Treatment in Emergency Department of Acute Heart Failure) study, a prospective observational cohort study of the management of patients presenting to the emergency for acute heart failure was published [1]. The one-liner conclusion – as summarized by tweets and online articles – was that early furosemide saves lives:
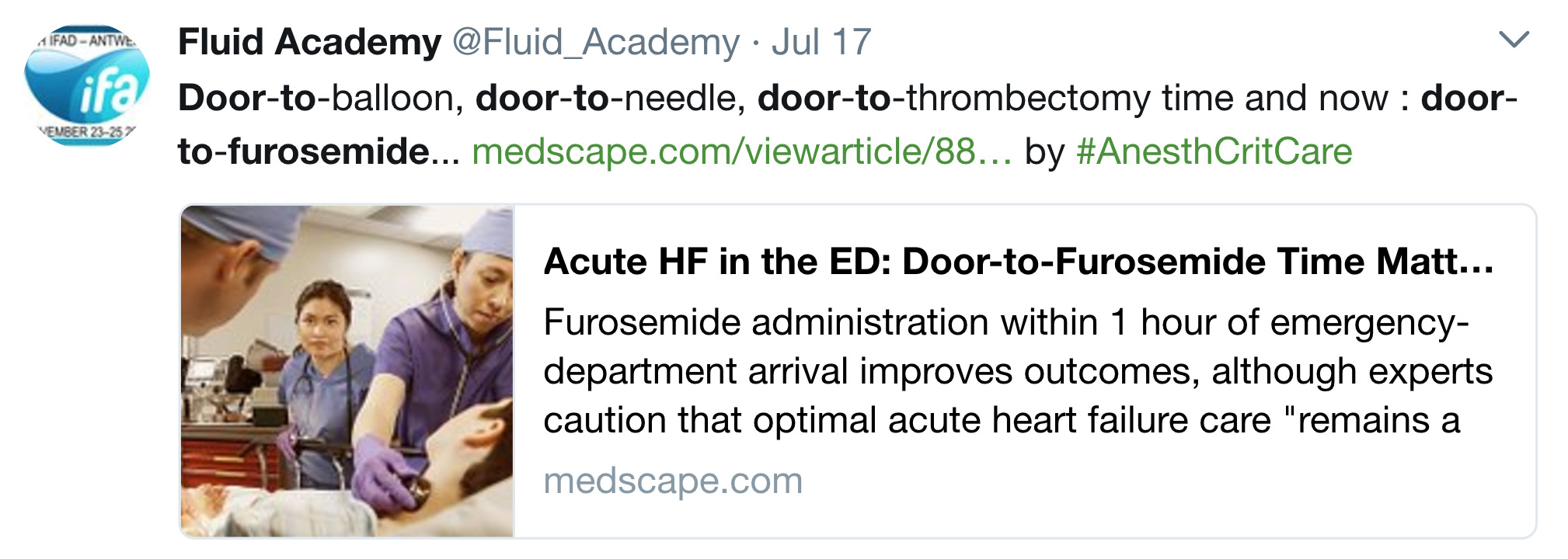
If early furosemide saves lives, why aren’t we giving it prehospital?
Because it doesn’t necessarily help and it has the potential to cause harm.
The REALITY- AHF was a prospective observational study that examined the association between door to furosemide (D2F) and all-cause-in-hospital-mortality. To be included in the study, patients had to be diagnosed with acute heart failure within their first three hours of admission to the ED. Patients who received furosemide within 60 minutes of arrival were assigned to the early treatment group. “Non-early” treatment was defined as furosemide administration at any time beyond the first hour. A total of 1291 patients met the inclusion criteria. 481 patients (37.3%) were classified as the early treatment group and 810 (62.7%) composed the non-early treatment group. Overall, the authors found a decrease in both in-hospital and 30-day mortality for patients who received furosemide within the first 60 minutes, (OR 0.36, 95% CI 0.19-0.71 and OR 0.52, 95% CI 0.28-0.96) respectively. Since the trial was not randomized, the authors attempted to control for confounding variables using propensity score matching and found similar results (OR 0.41, 95% CI 0.18-0.89 for in hospital mortality). The authors accounted for many variables – demographics, lab values – but not whether patients concurrently received therapies with proven outcome benefits such as nitroglycerin and ACE-inhibtors or Noninvasive Positive Pressure Ventilation( NIPPV )[2-5].
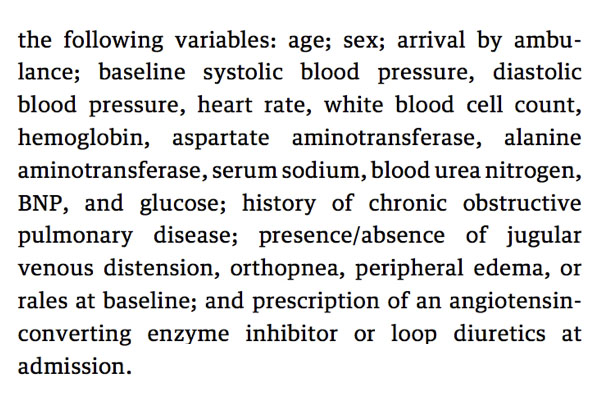
Variables accounted for in the Propensity Analysis by Matsue et. al. (Reference 1).
Patients who received earlier treatment were more likely to arrive by ambulance, had a more rapid onset of symptoms, and more severe congestive symptoms. As no other key interventions were examined – i.e. preload and afterload reduction – it is unclear whether “door-to-furosemide” time is simply a surrogate for the “door-to-rapid-recognition-and-treatment-of-acute-heart-failure” time.
The patients we care for in EMS are fundamentally different from the patients included in the REALTY-AHF study in one important way: they are undifferentiated. We care for patients with respiratory distress and shortness of breath, not an unequivocal diagnosis of acute heart failure. This is also true of the initial part of a patient’s stay in the emergency department. It is not always obvious at the time of presentation whether the etiology is acute heart failure, or rather a pulmonary embolism, Chronic Obstructive Pulmonary Disease (COPD), volume overload due to renal failure, sepsis from pneumonia or some combination of the above. Moreover, acute heart failure itself is not a homogenous disease. Most commonly heart failure is left-sided, but even then, it may be due to the heart’s decreased ability to pump blood into circulation (systolic heart failure) or incomplete filling during diastole [i.e diastolic heart failure or heart failure with preserved ejection fraction (HFpEF)]. Most emergency department patients with acute decompensated heart failure have preserved systolic function and are not overloaded in terms of total body volume [5]. Rather, these patients have a fundamentally vascular problem – one of an abrupt increase in afterload that results in acute decompensation. More importantly, although hypertensive, these patients may be euvolemic or even hypovolemic. In these cases, the treatment focuses on managing the flow of blood through system rather than eliminating fluid from the system. This is accomplished by NIPPV in the form of CPAP or BiPAP, high dose nitroglycerin, and ACE inhibitors [2-5].
Since many EMS and ED patients with acute decompensated heart failure are not volume overloaded, liberal use of diuretics may not be helpful and has the potential to be harmful [5]. Several studies have been published regarding prehospital furosemide administration, mainly examining the accuracy of paramedics’ working diagnosis of acute decompensated heart failure by comparing it to the final hospital diagnosis and studying the side effect profile and potential harm.
Jerome Hoffman and Susan Reynolds published a study in 1987 that evaluated the effect of prehospital furosemide on patient outcomes [6]. At the time of the study, paramedics in LA County were instructed to administer furosemide and morphine +/- nitroglycerin to patients with a clinical presentation consistent with pulmonary edema. Through clinical experience, the authors became concerned that morphine and furosemide led to clinically harmful respiratory depression and dehydration. They carried out a prospective sequential trial of therapies which included patients with shortness of breath as a presenting symptom and paramedic clinical suspicion for pulmonary edema and a SBP > 120. Patients received one of four treatment cocktails:
Group A: Sublingual nitroglycerin + 40 mg IV furosemide
Group B: 3 mg IV morphine + 40 mg IV furosemide
Group C: Sublingual nitroglycerin + 3 mg IV morphine + 40 mg IV furosemide
Group D: Sublingual nitroglycerin + 3 mg IV morphine [FUROSEMIDE-FREE]
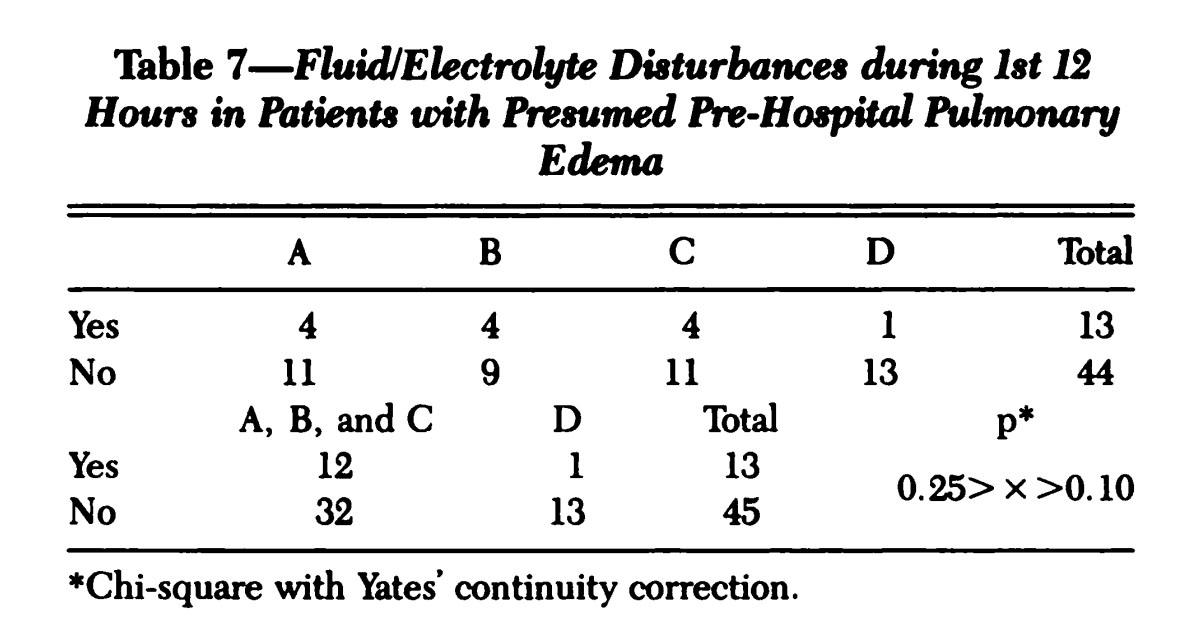
Table 7 from Hoffman and Reynolds (Reference 6) . Group D represents the “Furosemide-free” group.
Each therapy could be repeated up to three times and there were 15 patients in each group. As this was not an intention-to-treat analysis, 2 patients were excluded who did not receive the prescribed treatment. Patients were evaluated for clinical deterioration or improvement in the prehospital arena, in the emergency department, and 12 hours into their admission. The study found that only 77% of patients had pulmonary edema in the emergency department with the most common alternative diagnosis being COPD exacerbation. They also found that excluding nitroglycerin and administering morphine increased intubation rates. Finally, their data suggested that prehospital furosemide administration lead to complications including arrhythmias due to hypokalemia, hypotension, increased tachycardia and need for fluid administration without clear evidence of benefit. The authors concluded that prehospital pharmacologic treatment of respiratory distress due to pulmonary edema should be limited to nitroglycerin.
In contrast, a multi-center retrospective study by Pan et. al. (2014) failed to identify an association between prehospital furosemide administration and serious adverse events (acute renal failure, intubation, vasopressors or death) [7]. The study included acutely ill patients 50 years and older with dyspnea who were diagnosed with acute heart failure in either the prehospital or hospital record. 330 patients were subdivided into three categories: Furosemide without heart failure (N=58), furosemide with heart failure (N=110), and no furosemide with heart failure (N = 162). They performed a linear regression to identify whether there was an association between furosemide use and outcome. The adjusted odds ratio for serious adverse event for patients receiving furosemide was 0.62 (95% CI 0.33 – 1.43) for patients with heart failure and 1.14 (95% CI 0.58-2.23) in those without. Similar to the REALTY-AHF study, the adjustments accounted for historical factors, but not differences in use of NIPPV or nitroglycerin which differed significantly between the groups (see Table).
![Pan et. al. Table 3 [Reference 7]](/wp-content/uploads/2023/08/Pan_Table3.jpg)
Pan et. al. Table 3 [Reference 7]
34.8% of patients who received furosemide did not have a final ED diagnosis of acute heart failure. Other studies have found this proportion to vary anywhere between 15 – 36% [6-9]. This level of diagnostic accuracy is similar to emergency department physicians [10]. These represent a substantial proportion of critically ill patients who may be harmed by furosemide administration [9].
Take Home Points:
EMS cares for undifferentiated patients with shortness of breath. While expeditious furosemide therapy may benefit patients with acute heart failure due to volume overload, it may cause harm to the 15-36% of patients who are miscategorized as having acute decompensated CHF. EMS should continue to focus on appropriate use of therapies with significant benefit towards patient-centered outcomes, such as NIPPV, and leave consideration of door-to-furosemide time out of our protocols.
References
1. Matsue Y, Damman K, Voors A.A, et al. Time-to-Furosemide Treatment and Mortality in Patients Hospitalized With Acute Heart Failure. Journal of the American College of Cardiology Jun 2017, 69 (25) 3042-3051; DOI: 10.1016/j.jacc.2017.04.042
2. Sacchetti, A., Ramoska, E., Moakes, M. E., McDermott, P., & Moyer, V. (1999). Effect of ED management on ICU use in acute pulmonary edema. The American journal of emergency medicine, 17(6), 571-574.
3. Vital, F. M., Saconato, H., Ladeira, M. T., Sen, A., Hawkes, C. A., Soares, B., … & Atallah, Á. N. (2008). Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary edema. Cochrane Database Syst Rev, 3(3).
4. Levy, P., Compton, S., Welch, R., Delgado, G., Jennett, A., Penugonda, N., … & Zalenski, R. (2007). Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis. Annals of emergency medicine, 50(2), 144-152.
5. Scott, M. C., & Winters, M. E. (2015). Congestive heart failure. Emergency Medicine Clinics, 33(3), 553-562.
6. Hoffman, J. R., & Reynolds, S. (1987). Comparison of nitroglycerin, morphine and furosemide in treatment of presumed pre-hospital pulmonary edema. Chest, 92(4), 586-593.
7. Pan, A., Stiell, I. G., Dionne, R., & Maloney, J. (2014). Prehospital use of furosemide for the treatment of heart failure. Emerg Med J, emermed-2013.
8. Dobson, T., Jensen, J., Karim, S., & Travers, A. (2014). Correlation of paramedic administration of furosemide with emergency physician diagnosis of congestive heart failure.. Australasian Journal of Paramedicine, 7(3).
9. Wuerz, R. C., & Meador, S. A. (1992). Effects of prehospital medications on mortality and length of stay in congestive heart failure. Annals of emergency medicine, 21(6), 669-674.
10. Ackerman, R., & Waldron, R. L. (2006). Difficulty Breathing: Agreement of Paramedic andEmergency Physician Diagnoses. Prehospital Emergency Care, 10(1), 77-80.