Background: Peri-intubation hypoxia is an important quality measure for EMS agencies performing rapid sequence intubation, as it is associated with poor patient outcomes including peri-intubation cardiac arrest and death and poor neurologic outcome following traumatic brain injury. The aim of this study was to determine if implementation of a “clinical bundle encompassing positioning, apneic oxygenation, delayed sequence intubation and goal-directed pre-oxygenation is associated with decreased peri-intubation hypoxia compared with standard out-of-hospital rapid sequence intubation.”
Methods: This was a retrospective before-and-after study utilizing data from Williamson County EMS in Texas. Williamson County EMS is a suburban EMS system that staffs Paramedic-Paramedic, utilizes the King Vision video laryngoscope for intubation, has regular training in airway management and a baseline first pass intubation success rate of 85%. The study included all adult non-arrest patients requiring intubation. The primary outcome of interest was the proportion of patients with peri-intubation hypoxia, defined as an oxygen saturation < 90% occurring at any time during intubation attempts.
In the “before period”, the agency used standard rapid sequence intubation approach for non-cardiac arrest patients consisting of NRB, ketamine + paralytic, apneic oxygenation and intubation. Following a training and implementation period, the agency implemented a clinical bundle consisting of the following components: ketamine administration (without paralytic), BVM+PEEP and NC oxygenation, patient positioning (head up/ear to sternal notch), minimum of 3 minutes of an SpO2 of > 93%, followed by paralytic administration and intubation. If they were unable to achieve an acceptable pre-intubation SpO2, a supraglottic airway was inserted. The clinical bundle required the second paramedic to act as an observer and timer.
Physiologic events were measured by manual review of monitor data, including continuous waveform capnography and pulse oximetry. Patients were excluded from the analysis if they had incomplete pulse oximetry data or if in the after group, the clinical bundle was initiated but intubation was not attempted secondary to inability to meet pre-oxygenation goals (18/105 patients, 17%).
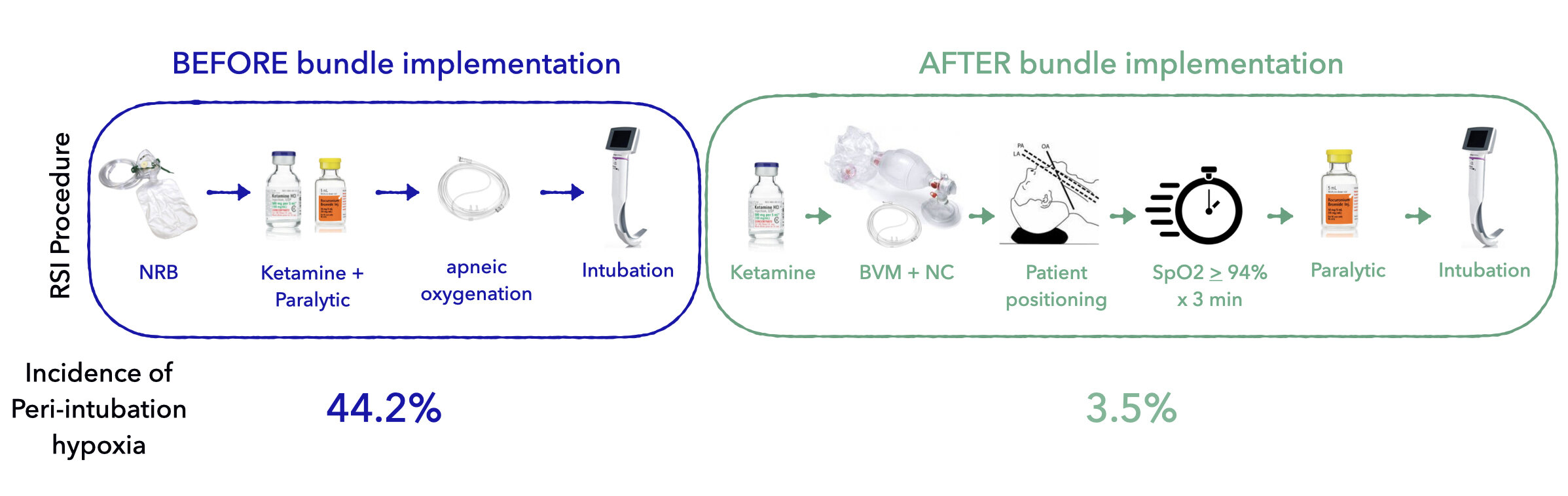
Key Results: The study included 104 patients in the before group and 87 patients in the after group. The before and after groups were not significantly different in terms of initial hypoxia (40.4% vs. 41.4%), first pass success (84.6% vs. 88.5%) or overall success (95.2% vs. 93.1%). However, the rate of peri-intubation hypoxia dropped significantly (44.2% vs. 3.5%). The median scene time increased by 9 minutes (95% CI 5.0 to 13.0 minutes) following bundle implementation. Even if you include the 17% of patients who were excluded for the “After” group for failure to meet pre-oxygenation goals, this represents a significant improvement. There was no difference in incidence of peri-intubation cardiac arrest, but the study was not powered to detect a difference in this low frequency event.
Conclusions: Implementation of a “clinical bundle emphasizing patient head positioning, apneic oxygenation, delayed sequence intubation, and goal-directed pre-oxygenation” has the ability to decrease the rate of peri-intubation hypoxia in non-cardiac arrest patients undergoing rapid sequence intubation.
What This Means for EMS: This study is an excellent potentially practice-changing study that blurs the lines between improvement science and research. EMS providers, agency leadership, and medical oversight should be monitoring incidence of patient-oriented quality measures such as peri-intubation hypoxia to ensure quality of care of delivery. Implementation of clinical care bundles and processes geared at improving performance on such measures have potential to greatly improve patient care.
Article Summary by Maia Dorsett, MD PhD FAEMS