Article Bites Summary by Kristopher Bianconi, MD
Background
The administration of medications to pediatric patients complex, with some medications having error rates as high as 60% in the prehospital setting. Converting a patient’s weight from pounds to a dose based on mg’s/kg creates a dizzying dance with math made more difficult by the stress of providing prompt and appropriate pediatric critical care. The introduction of physical and electronic portable medication guides work to help ease this burden with the primary goal of reducing medication dosing errors. The NAEMSP has a position statement and resource document regarding medication dosing safety for pediatric patients.
Methods
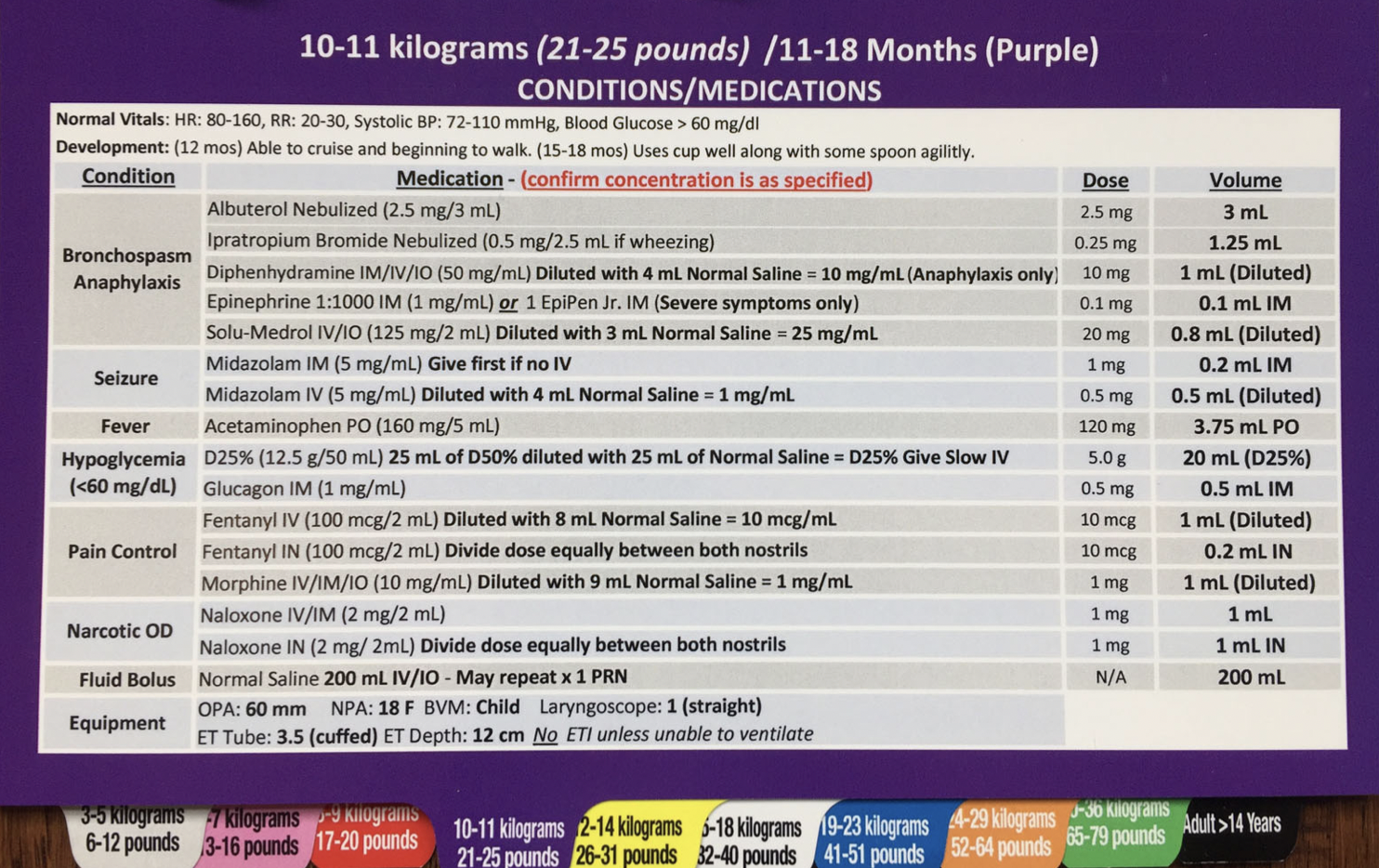
MI-MEDIC PDR. Image from this study.
This was an observational study of paramedics from 15 EMS agencies throughout the state of Michigan. Using the MI-MEDIC pediatric dosing reference (PDR), paramedics have available an on-scene instruction binder on appropriate medication dose in milliliters based on the patient’s weight. For medications which require dilution prior to administration, the PDR has a step-by-step guide to preform dilution correctly. To test its efficacy, paramedics were run through a series of simulations which were recorded and reviewed by study investigators to evaluate for medication dosing errors. These results were then compared to prior simulation evaluations from the same agencies to evaluate if the PDR reduced the error rate.
The teams participating in the simulations were a mix of two paramedic providers, a paramedic with an EMT-I, or a paramedic with an EMT-B. In the two paramedic teams, one was elected to calculate, draw up, and administer the medication individually, while in the mixed teams the paramedic is the only practitioner qualified to work with the medications. They were asked to preform four simultaneous pediatric simulation cases; an infant having a hypoglycemic seizure, an 18-month old patient with burns, a 5 year old with anaphylaxis, and an infant in cardiac arrest. Each case was preformed sequentially, simulated guardians were present during the cases, and the PDR was available to all paramedics during each simulation allowing them to reference it as often as needed.
Results
A total of 36 crews participated, allowing for 142 simulations to be evaluated. Overall, paramedics in this study were able to administer medications appropriately to pediatric simulation patients 68.8% of the time. This ranged from a high of correct diphenhydramine dose at 82.8% to a low of correct Midazolam IV dose at 38.9%. Compared to data obtained prior to the implantation of the PDR, correct dose rates increased by at least 30% for IM midazolam, Dextrose, and IM or IV Epinephrine.
Observed errors included both over and under doses, the most common overdoses occurred with IV epinephrine with 13 overdoses, IV fentanyl with 16 overdoses, and IV Midazolam with 8 overdoses. The most common underdoses noted were IV epinephrine with 6 underdoses, IM Midazolam with 9 underdoses, and IV Dextrose with 5 underdoses. Particular to epinephrine IV, there were six 10-fold overdoses with one 10-fold under doses after the medication was erroneously diluted. When examining the effect of dilution, the authors note a decrease in correct dose administration rate of 26.7% when giving IV midazolam, which must be diluted, compared to IM Midazolam, which may be given as is. Finally, in all but three cases the paramedics established the patient’s appropriate weight-based dosing, most often via Broselow tape, followed by asking simulated guardians the patient age and/or the patient’s weight.
Conclusions
In this study the use of a PDR was associated with an increase in the success rate of correct medication dose administered during simulation of critical pediatric patient encounters. Despite its presence, there was still an overall error rate greater than 30% with multiple overdoses of medications well known to depress respiratory drive being noted. The introduction of similar tools in other mobile health systems is likely to be of help in reducing the rate of medication errors for paramedics, however further work needs to be done to get error rates within ranges we can all be more comfortable with.
References
Hoyle JD Jr, Ekblad G, Hover T, Woodwyk A, Brandt R, Fales B, et al. Dosing errors made by paramedics during pediatric patient simulations after implementation of a state-wide pediatric drug dosing reference. Prehosp Emerg Care Mar-Apr 2020;24(2):204-13.
Editing by Jeremy Lacocque, DO and James Li, MD